Characteristics of the Study Cohort: A Deep Dive
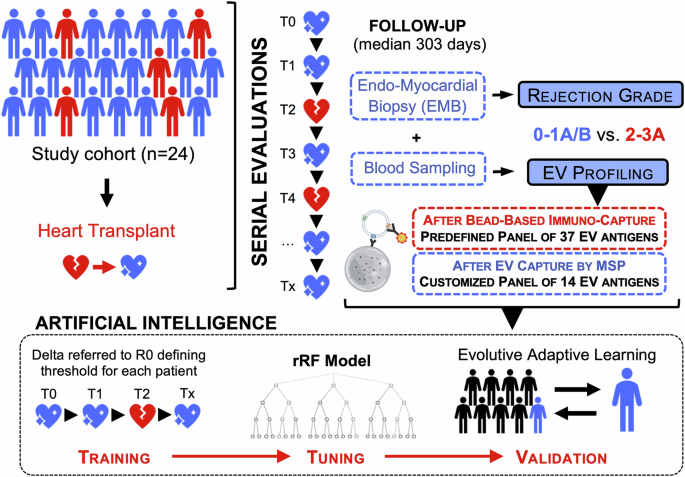
In recent advancements in heart transplantation, understanding the intricacies of patient characteristics is crucial. This article explores the details of a prospective cohort study involving 24 consecutive heart transplant patients, offering insights into their demographics, clinical evaluations, rejection episodes, and the innovative use of extracellular vesicles (EVs) for monitoring.
The Patient Demographics
This cohort comprised 24 patients who had all undergone heart transplantation at the same referral center using standardized protocols. The median follow-up period for these patients was 303 days, with each patient attending between 9 to 17 scheduled visits. Notably, the mean age of participants was 58 years, and an overwhelming 83.3% were male, indicating a demographic trend that leans towards middle-aged males in heart transplant cases.
At their first post-transplant visit, the recipients presented as normotensive, with a mean Body Mass Index (BMI) of 24.7 kg/m². While the renal function was mildly reduced (mean estimated Glomerular Filtration Rate – eGFR = 65 mL/min), both left and right ventricular functions were preserved, showcasing the initial success of the transplant.
Interestingly, only one patient (4.2%) reported mild dyspnea, categorizing him under NYHA class II, which suggests that the majority of the patients enjoyed a relatively symptom-free early recovery stage.
Clinical Assessments and Rejection Episodes
Throughout the longitudinal follow-up, the patients underwent various evaluations at each visit. These included clinical evaluations, biochemical exams, blood sampling, and endomyocardial biopsies (EMB), culminating in a total of 285 assessments.
The findings documented 181 instances of grade 0 rejection and 104 episodes of acute cellular rejection (ACR). Of the episodes classified as ACR, 28.1% were grade 1A/B, 3.5% grade 2, and 4.9% grade 3A. Notably, 14 of the 24 patients experienced grade 2-3A rejections, with three individuals having multiple episodes. This high rate of rejection highlights the ongoing challenges that transplant patients face post-procedure.
In terms of symptomatic presentations during rejection episodes, a remarkable 91.7% of patients remained asymptomatic during grade 2-3A ACR, while only a single individual exhibited dyspnea. Such data suggest that ACR can often occur silently, requiring intricate monitoring to detect changes before they manifest visibly.
Biochemical and Immunosuppressive Profiles
Further assessing the biochemical parameters, it was observed that patients exhibited higher levels of monocytes and basophils associated with grade 3A ACR. However, other white blood cell populations and indices related to liver and renal function showed no significant variations.
Across the different rejection grades, patients maintained uniform immunosuppressive regimens. Common medications included cyclosporine, prednisone, mycophenolate, azathioprine, tacrolimus, and/or everolimus. These findings prompt discussions regarding the adequacy of current immunosuppressive protocols in preventing graft rejection.
Exploring Molecular Insights: The Role of EVs
To further refine rejection monitoring, researchers employed profiling of circulating extracellular vesicles (EVs). This innovative approach involved the collection of plasma samples from patients for assessing the presence of immune antigens. Utilizing an indirect flow cytometric method, the study identified 14 differentially expressed EV antigens that exhibited progressive increases in levels corresponding with the severity of ACR.
This not only provides a clearer molecular picture of the rejection process but also emphasizes the role of EVs as putative biomarkers for real-time monitoring. Notably, the successful identification of these EV markers substantiates their potential as early indicators of rejection, preceding conventional histological assessments.
Advancements in Predictive Modeling Through AI
Utilizing artificial intelligence (AI) further enhances the prognostic capabilities of EV profiling. A model developed based on supervised learning algorithms can discern ACR by interpreting unique EV fingerprints associated with different rejection grades. This model dynamically adjusts to individual patient profiles, thereby improving its sensitivity in predicting acute rejections.
The AI model demonstrated remarkable diagnostic performance, showcasing high accuracy across various testing cohorts. The likelihood of rejection escalated significantly with increasing EV marker levels, indicating a noteworthy correlation between the data derived from EV analysis and clinical outcomes.
Correlations and Clinical Implications
The intricacies of the findings reveal a lack of significant correlations between EV markers and traditional biochemical profiles, proposing that EV signatures may be more responsive to rejection episodes than conventional metrics. Furthermore, multivariate regression models indicated that the profiling of EV antigens was independently associated with ACR, regardless of the immunosuppressive regimen.
Notably, the AI model showcased its dynamic capability by accurately predicting a patient’s rejection status and adjusting treatment accordingly. This adaptability highlights the importance of integrating advanced technologies into clinical practice, potentially enhancing patient management strategies in heart transplantation.
As the field of heart transplantation continues to evolve, the characteristics of patient cohorts and the integration of novel monitoring techniques, such as EV profiling and AI predictive models, pave the way for improved patient outcomes. The future holds promise for these insights to redefine therapeutic approaches, emphasizing personalized patient care in transplantation medicine.