Understanding Steatotic Liver Disease: A Comprehensive Guide
Steatotic Liver Disease (SLD), previously known as fatty liver disease, represents a significant health concern characterized by the accumulation of fat, or steatosis, in over 5% of the liver’s hepatocytes. Recent advancements in nomenclature have led to the classification of SLD into five distinctive groups: Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), Alcohol-Associated Liver Disease (ALD), a combination of both (MetALD), SLD secondary to specific etiologies, and cryptogenic SLD. This reclassification helps to clarify the various causes of liver disease and enhances diagnostic accuracy.
The Rise of MASLD
MASLD has emerged as the most prevalent cause of chronic liver disease globally, largely linked to rising rates of diabetes, obesity, and metabolic syndromes. Recent estimates suggest that around 30-38% of adults are affected, reflecting a worrying growth of 50.4% over the past 30 years. Intriguingly, regions like South America report even higher prevalence rates, reinforcing the urgent need for awareness and intervention.
Particularly concerning is MASLD’s widespread occurrence in metabolic risk groups. Studies indicate that over 70% of patients with type 2 diabetes mellitus (T2DM) and a staggering 90% of severely obese individuals undergoing bariatric surgery are nursing this condition. In contrast, ALD maintains a relatively stable global prevalence of about 8%, with alcohol consumption remaining one of the leading causes of chronic liver disease.
Complications and Comorbidities
The implications of SLD extend beyond liver health. The disease can progress to steatohepatitis, fibrosis, cirrhosis, and even hepatocellular carcinoma (HCC). Such progression is alarming, especially considering the increase in all-cause mortality associated with SLD. Importantly, both MASLD and ALD have been identified as leading indications for liver transplantation.
Moreover, individuals with MASLD are at a heightened risk for various comorbid conditions. Evidence suggests a relationship between MASLD and non-liver malignancies, cardiovascular disease, cognitive impairments, and chronic kidney diseases. This multifaceted relationship underscores the complex interplay between liver health and systemic wellbeing.
Economic Impact of SLD
The financial burden arising from SLD is substantial and growing. Patients diagnosed with MASLD see up to a 40% increase in outpatient visits over five years compared to their non-MASLD counterparts. Healthcare costs linked to MASLD are noticeably higher, further emphasizing the need for early diagnosis and intervention. Alarmingly, deaths associated with MASLD complications, such as cirrhosis and liver cancer, have escalated significantly over the past few decades.
Diagnosing SLD: Current Approaches
Diagnosing SLD typically involves evidence of hepatic steatosis, which can be identified through imaging or histology. While liver biopsy remains the gold standard, it carries certain risks and is generally reserved for complex cases. Instead, radiological methods are commonly employed, with abdominal ultrasound being the first-line diagnostic tool.
Ultrasound is favored for its accessibility and relative safety, presenting a good sensitivity and specificity for detecting liver abnormalities. Despite this, it has its limitations, particularly in patients with obesity or mild steatosis. More advanced imaging techniques like magnetic resonance spectroscopy (MRS) or magnetic resonance proton density fat fraction (MRI-PDFF) are more accurate but come at a higher cost.
The Challenge of Early Detection
One of the primary challenges in managing SLD is its often asymptomatic nature, particularly in early stages. This necessitates the development of effective screening strategies to identify at-risk individuals before significant damage occurs. Current recommendations suggest screening for individuals displaying features of metabolic syndrome.
Unfortunately, adequate screening methodologies are not universally accessible, particularly in primary care settings. Therefore, there is an ongoing effort to create predictive models that rely on clinical and biochemical variables, which could enhance early detection without the need for invasive procedures.
Advances in Predictive Modeling
Recent advancements in machine learning (ML) present exciting avenues for improving SLD diagnosis. Numerous models have been created to predict liver disease using various clinical variables, including age, BMI, and liver enzyme levels. Some models even incorporate lifestyle factors to enhance predictive accuracy.
A variety of ML techniques like random forests and extreme gradient boosting have been explored, with differing success rates. Notably, using combinations of variables, such as triglycerides, glycemia, and abdominal circumference, has shown promise in optimizing prediction outcomes.
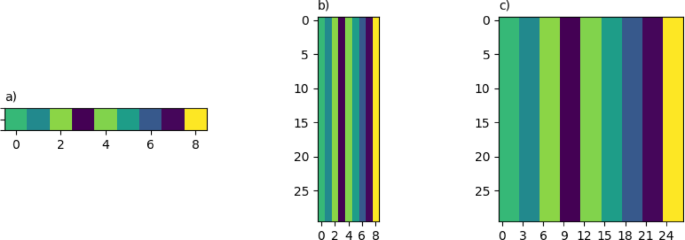
Deep learning (DL) represents the next frontier in this domain. By transforming tabular data into images, DL models can leverage CNN architectures designed for pattern recognition. Such innovations aim to enhance classification capabilities, ultimately leading to improved predictive performance over traditional ML models.
Innovative Methodologies and Findings
Research has reported significant strides in developing DL methods for SLD prediction. These novel approaches convert clinical data into images, allowing CNNs to identify complex patterns that traditional models may miss. Such innovations draw inspiration from the way human cognition analyzes visual data, bringing a fresh perspective to medical data interpretation.
This evolving approach has yielded promising results, demonstrating improved accuracy in predicting SLD by reducing false positives while maintaining sensitivity levels. The implications of such advances could be transformative, especially for a disease that affects millions globally.
Future Directions
With an increasing emphasis on early diagnosis and treatment strategies, future research will likely continue to pivot toward enhancing predictive accuracy using sophisticated modeling techniques. As both the understanding of SLD and the tools available for managing it advance, the integration of ML and DL into clinical practice may facilitate a more robust response to this rising public health concern.
Given the intricate relationships between SLD, metabolism, and wider health issues, fostering a holistic approach that addresses not only liver health but overall well-being remains essential. In this context, continued collaboration among healthcare providers, researchers, and patients will be crucial in shaping a proactive future for SLD management and intervention strategies.