Revolutionizing Mental Health Care with Generative AI
Revolutionizing Mental Health Care with Generative AI
Understanding Generative AI in Mental Health Care
Generative AI refers to algorithms that can create content, including text and images, based on input data. In mental health care, this technology has the potential to transform how practitioners personalize treatment and improve patient outcomes. Researchers are beginning to harness this tool to address gaps in care accessibility and cultural competence.
For example, a recent study by a team at the University of Illinois Urbana-Champaign simulated the mental health journey of a fictional patient named “Marcus Johnson.” This composite character was designed to reflect the experiences of a young, middle-class Black man facing depression. The researchers used generative AI to craft a personalized treatment plan based on Marcus’s circumstances, highlighting barriers such as cultural expectations and the availability of culturally sensitive care.
Key Components of Generative AI Frameworks
Three essential components define the use of generative AI in this context: clinical modeling, access frameworks, and measurement-based care. Clinical modeling involves creating simulated patient scenarios that reflect real-world challenges. Access frameworks evaluate the availability and acceptability of mental health services, while measurement-based care utilizes standardized tools for assessing ongoing patient progress.
In the Illinois study, researchers implemented these frameworks to ensure that Marcus Johnson’s treatment plan was not only theoretically sound but also applicable in real-world settings. This multi-faceted approach allows practitioners to tailor their methods and understand the diverse needs of their clients.
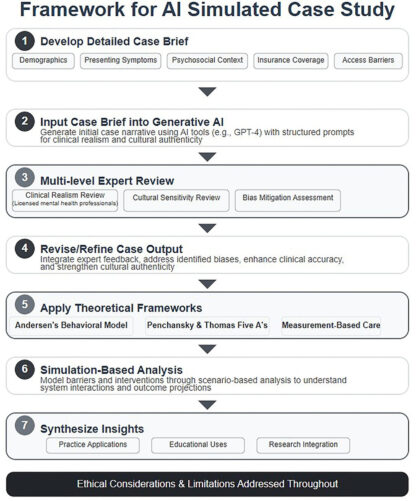
The Process of Implementing Generative AI in Therapy
Using generative AI in mental health treatment involves a step-by-step process. First, researchers and practitioners create a composite patient profile, incorporating demographic factors and potential barriers to care. Next, the AI generates a simulated treatment plan that reflects the patient’s unique conditions and cultural context.
After the AI produces its recommendations, licensed mental health professionals review these outputs to ensure clinical accuracy. This review process is crucial, as it aligns AI-generated solutions with established mental health practices. Importantly, using simulated patients minimizes privacy concerns while facilitating the exploration of innovative intervention strategies.
Real-World Applications: A Mini Case Study
In a concrete application, the Illinois team examined Marcus Johnson’s case by prompting the AI with various frameworks, including Andersen’s Behavioral Model, which studies health services utilization. Through this model, they unearthed both facilitating and hindering factors affecting Marcus’s access to care. This real-world simulation not only provides a template for individualized treatment but also helps educators and clinicians understand community-specific barriers.
The findings underscore the need for culturally competent care strategies, as the issues faced by Black men in the U.S. healthcare system can significantly affect treatment outcomes. This approach serves as a valuable teaching tool for future clinicians, ensuring they are aware of the complexities surrounding mental health in diverse populations.
Common Pitfalls and How to Address Them
Integrating generative AI into mental health care is not without challenges. One critical pitfall is the risk of generating recommendations that lack cultural relevance or fail to account for systemic barriers. This misalignment can lead to ineffective treatment modalities that may reinforce existing disparities.
To mitigate these risks, it is vital to involve mental health professionals in the review process. Their expertise ensures that AI-generated suggestions are grounded in real-world experiences and cultural nuances. Regular calibration of the AI’s underlying data sets can also enhance its responsiveness to the changing landscape of mental health needs.
Tools and Frameworks in Practice
Several frameworks and tools facilitate the effective use of generative AI in mental health settings. For instance, the Measurement-Based Care framework provides practitioners with metrics to evaluate client progress continually. This approach allows for data-driven adjustments to treatment plans, ensuring their effectiveness over time.
However, while generative AI shows promise, practitioners must recognize its limitations. The effectiveness of AI outputs relies heavily on the quality of the data used in training models. As noted by the study’s authors, AI-generated content may not capture the emotional and contextual nuances necessary for effective mental health care.
Alternatives to Generative AI
While generative AI presents significant opportunities, other models and technologies may also complement mental health treatment. Traditional therapy methods, including cognitive-behavioral therapy (CBT) and community-based support programs, offer robust frameworks that address individual psychological needs.
Choosing between generative AI and more conventional approaches hinges on the specific requirements of the patient population. Generational differences, cultural backgrounds, and access to care resources may inform which strategy is most beneficial in different contexts.
FAQ
Can generative AI replace traditional therapists?
No, while it can enhance treatment planning and education, human therapists are essential for emotional connection and nuanced decision-making.
Is generative AI safe for all patient populations?
Generative AI’s safety varies; it can be beneficial but must be carefully monitored to ensure cultural and contextual relevance.
What are possible future developments in this area?
As datasets expand and methodologies improve, generative AI could provide even more tailored treatment strategies that enhance overall care delivery.
How does generative AI impact student training?
It equips students with practical, evidence-based scenarios to better prepare them for real-world challenges in diverse mental health contexts.