Predicting Mental Health Problems Using Deep Learning and Brain Structure
Introduction to Deep Learning in Mental Health
The intersection of artificial intelligence (AI) and mental health is an emerging field that holds promise for understanding and addressing the complexities of mental health disorders. Recent research examines the utility of deep learning to predict mental health issues based on measures of brain structure. These methods offer insights beyond traditional regression approaches, potentially uncovering significant neurobiological markers associated with internalizing problems in children and youth.
Study Overview: Cross-Sectional Insights
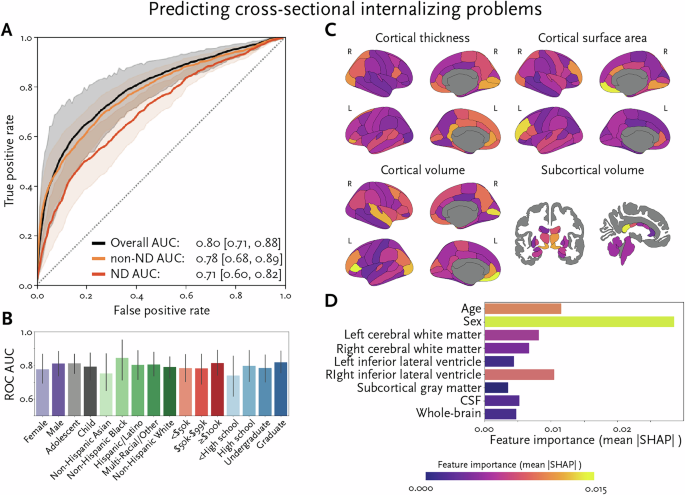
In a groundbreaking study involving over 14,500 children and youth, deep learning achieved a mean Area Under the Curve (AUC) score of 0.80 when predicting internalizing problems. This high performance underscores the capability of AI to analyze neurobiological data, revealing patterns that traditional methods may overlook. While these findings offer extensive insights into the neurobiology underlying mental health issues, the cross-sectional nature of the study suggests that direct clinical applications may be limited.
Importance of Symptom Measures
Interestingly, the study emphasizes the potential benefits of using symptom measures over traditional diagnostic labels as prediction targets. As AI technology evolves, it has shown considerable promise in diagnosing neurodevelopmental conditions like autism and ADHD based on neurobiological data. However, these conditions exhibit significant heterogeneity, complicating predictive accuracy.
Challenges with Longitudinal Predictions
While the cross-sectional model performed optimally, its longitudinal counterpart, which involved over 10,500 children and youth from the general population, achieved a lower AUC score of 0.66. This indicates that predicting worsening trajectories of mental health issues over time remains challenging, especially in a representative sample. However, the model fared better when tested with an external dataset primarily composed of neurodivergent youth, where the AUC score rose to 0.80.
Neurodivergence and Predictive Capacity
The model showed promise for individuals diagnosed with neurodevelopmental disorders, achieving a mean AUC of 0.73 across the broader sample. This difference sheds light on the potential of deep learning to identify youth at high risk for worsening mental health trajectories, particularly among those with neurodevelopmental diagnoses.
Biological Foundations of Mental Health
The effectiveness of the model suggests that biological differences linked to neurodevelopmental disorders may provide more accurate predictions of mental health challenges. Ongoing debates in the field raise questions about whether these difficulties stem from shared mechanisms among neurodivergent individuals or if they are fundamentally distinct from those observed in the general population.
Unique Neuroanatomical Features
The study identified key neuroanatomical features predictive of internalizing problems, primarily concentrated in the prefrontal cortex, temporal poles, and corpus callosum. These regions have established roles in emotional processing and regulation, indicating that their structural characteristics may reflect vulnerabilities that predispose individuals to mental health issues.
The Role of Sex in Predictions
Sex emerged as a significant variable in both the cross-sectional and longitudinal models. Surprisingly, the findings indicated that being male increased the likelihood of having internalizing problems in the cross-sectional model. In contrast, being female was linked to a higher probability of worsening problems in the longitudinal model. This duality highlights the complex role of sex in mental health trajectories, suggesting that traditional views on gender differences may need reevaluation.
Advancements in Predictive Models
The use of deep learning models allows for a nuanced understanding of the relationship between brain structure and mental health, capturing intricate patterns that traditional statistical methods may miss. The findings reveal that certain regions are not just correlates but may actually encode vulnerability or resilience in response to mental health challenges.
Implications for Clinical Practice
These insights have far-reaching implications for the development of tailored interventions. By identifying biological markers associated with mental health trajectories, healthcare providers can offer timely and personalized care, potentially mitigating the rising burden of mental health issues on families and healthcare systems.
Limitations and Future Directions
While the study is promising, it is not without limitations. It primarily focused on brain structural measures, leaving out other neurobiological factors such as functional connectivity and genetic influences. Additionally, the reliance on caregiver reports for assessing internalizing problems may introduce biases, and the age constraints of the sample limit generalizability across developmental stages.
Broader Applications and Community Involvement
Future research should aim to include diverse neurobiological measures and explore the prediction of various types of mental health problems. It will be crucial to involve both clinicians and the neurodivergent community in designing studies and interventions to ensure the acceptability and relevance of these tools in real-world settings.
Conclusion: Towards Personalized Mental Healthcare
In summary, this study highlights the potential of deep learning and neurobiological measures in predicting mental health problems among children and youth. As the field evolves, there is significant promise in using AI-driven insights to tailor interventions and support systems, ultimately enhancing mental health outcomes for vulnerable populations.