Exploring the Use of Machine Learning for Predicting Bloodstream Infections
In the landscape of modern medicine, machine learning (ML) stands out as a transformative tool, especially in predicting complex health conditions like bloodstream infections (BSI). Our recent investigation into the feasibility of utilizing ML models primarily based on biochemical variables reveals important insights into their performance and potential applications.
The Challenge of Detecting Bloodstream Infections
Bloodstream infections are a significant concern in healthcare, particularly among critically ill patients. With up to 50% of intensive care admissions involving an infection, effective identification and management of BSI are crucial. However, the confirmation of infections through microbiological samples can be challenging due to the prevalence of broad-spectrum antibiotics used in such settings. Historically, various biochemical markers—like C-reactive protein (CRP), procalcitonin (PCT), and leukocyte counts—have emerged as possible indicators for diagnosing BSI.
Model Performance: A Mixed Bag
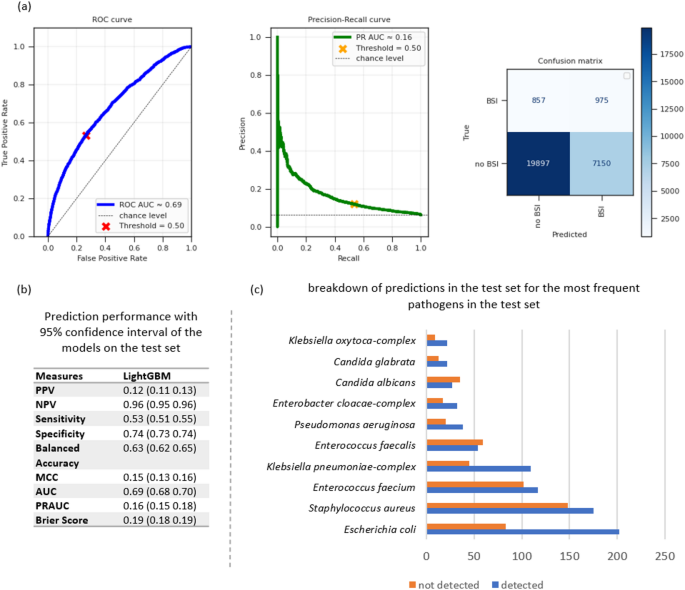
Our findings indicate that the ML models we implemented showcase poor to moderate performance regarding the identification of BSI cases. Specifically, the best-performing model achieved a positive predictive value (PPV) of only 0.12. Despite this, the model showed promise as a rule-out tool due to its notably high negative predictive value (NPV) of 0.96 and a specificity of 0.74. This ability to effectively identify negative cases signifies the model’s potential role in preventing unnecessary antibiotic treatments and hospital costs while promoting responsible antibiotic administration.
Interestingly, when zooming in on certain clinically relevant pathogens—such as Staphylococcus aureus, Escherichia coli, and Enterococcus faecium—the model demonstrated elevated precision (0.66). This suggests that while the overall predictive capability may be limited, the model can still pinpoint certain infections more accurately.
Key Biochemical Contributors
A closer look at the model’s contributions revealed that platelets emerged as the most significant predictor of BSI, followed closely by leukocytes, the neutrophil-to-lymphocyte ratio, monocytes, and CRP. The pronounced impact of platelets is particularly noteworthy; despite their relatively understudied role in BSI prediction, they could become a focal point for future investigations. The study aligns with prior research, which emphasizes the importance of these biochemical markers in identifying the risk of infections.
Understanding Patient and Pathogen Dynamics
Our study focused on a diverse patient population, including immunocompromised individuals and those admitted for varying reasons. This complexity highlights the challenge of predictive modeling in BSI. Factors such as underlying health conditions, treatment history—including antibiotic use—and environmental elements all contribute to the difficulty of establishing accurate predictions based solely on biochemical data.
Moreover, the model’s lower predictive performance may also reflect the data quality and completeness issues, especially when it comes to information on other risk factors like catheter-related treatments or vital signs, which can significantly influence diagnosis.
The Importance of External Data and Future Directions
While the study benefited from a robust dataset spanning over a decade with 144,398 instances from 54,188 patients, we noted the pressing need for external validation of our model. Incorporating external datasets can help enhance the generalizability and applicability of our findings. Furthermore, examining specific cohorts—such as transplant recipients or those with particular bacterial infections—could refine the predictive capabilities and sensitivity of ML models.
The study also identified essential areas for future exploration, particularly in enriching the dataset with additional clinical parameters, such as vital signs and invasive procedures. Accounting for these variables could improve sensitivity and provide a more holistic view of patient states.
Ethical Concerns and Risk Assessment
Another important aspect to consider is the ethical implications of using ML for BSI prediction. False-negative blood cultures are a known issue, which could undermine the model’s reliability. Integrating additional diagnostic tools like PCR-based assays might help mitigate the risk of inaccurate readings and enhance the overall performance of predictive models.
Moreover, as the focus broadens toward public health and antibiotic resistance, combining ML with epidemiological data opens new avenues for addressing these growing concerns.
Leveraging Machine Learning in Routine Care
Our exploration into using biochemical markers for early BSI prediction aligns with broader trends in ML applications in healthcare. The methodology we employed offers a systematic approach to identify potential biomarkers for bloodstream infections and highlights the significant role machine learning can play in urgent clinical settings.
While the current predictive capabilities indicate that ML models may be best suited for ruling out BSI cases, further refinement and validation hold the potential to enhance their value in clinical workflows. With the goal of delivering near real-time results, ML can play a vital role in recognising and responding to infection risk—contributing to improved patient outcomes in hospital settings.