“Interpretable Deep Learning Model Identifies Gastrointestinal Stromal Tumors and Lesion Features via Microprobe Endoscopic Ultrasonography”
Interpretable Deep Learning Model Identifies Gastrointestinal Stromal Tumors and Lesion Features via Microprobe Endoscopic Ultrasonography
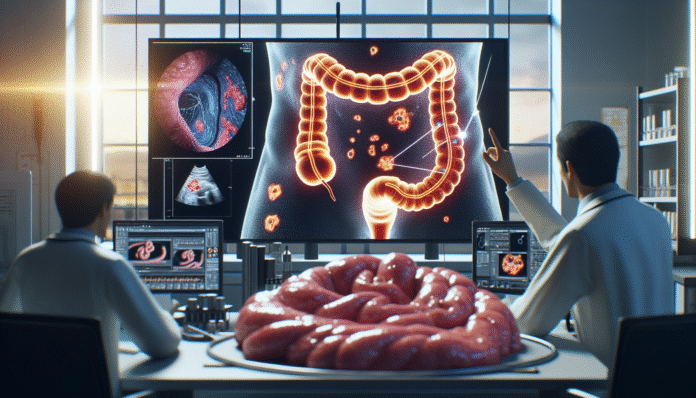
Deep learning, a subset of artificial intelligence, refers to algorithms structured in layers to analyze data through various levels of abstraction. One noteworthy application of this technology is in the diagnosis of gastrointestinal stromal tumors (GISTs), a type of tumor that occurs in the digestive tract. The recent development of an interpretable deep learning model aims to enhance the accuracy of diagnosing GISTs and identifying lesion characteristics using microprobe endoscopic ultrasonography (MEUS), a technique that provides high-resolution images from within the gastrointestinal tract.
Core Concept and Its Significance
GISTs are rare tumors that often pose challenges in diagnosis due to their subepithelial location. Accurate identification often requires advanced imaging techniques, such as MEUS, which provides detailed views of the lesions. This deep learning model not only diagnoses these tumors but also provides interpretable data that assists doctors in making informed decisions. The implications of this advancement are far-reaching, potentially improving patient outcomes and streamlining treatment processes by facilitating early and accurate interventions.
Key Components of the Model
The model leverages critical tumor features from MEUS images, such as the originating layer, echogenicity (the ability of tissues to reflect ultrasound waves), and echo heterogeneity (variability in the echogenic response). Each of these aspects contributes essential data necessary for an accurate diagnosis. For instance, a GIST typically exhibits specific echogenic patterns that set it apart from other types of lesions, such as leiomyomas or schwannomas. By focusing on these key components, the model enhances diagnostic precision, reducing the likelihood of misdiagnosis.
Step-by-Step Process
Developing this deep learning model involved several strategic stages. Initially, a training set of 522 subepithelial lesions (SELs) was compiled from various hospitals. The data collection process emphasized the importance of quality control; only images deemed satisfactory by experienced endoscopists were used.
Next, the research team developed multiple AI models, each incorporating different combinations of lesion characteristics. A crucial step involved validating these models using a separate set of images to determine which configuration yielded the best performance. Ultimately, the model with the highest receiver operating characteristic curve (ROC AUC) was selected for further evaluation, demonstrating its potential effectiveness across diverse clinical settings.
Practical Examples of Implementation
In practical settings, the interpretable deep learning model has demonstrated significant accuracy in distinguishing GISTs from other SELs. For example, during clinical trials, the model showed a high predictive score that correlates with the assessment conducted by seasoned endoscopists. This collaboration between AI diagnostic tools and human expertise highlights how technology can bolster clinical practice, particularly in complex diagnoses.
Common Pitfalls and Their Solutions
While the integration of deep learning in medical diagnostics is promising, potential pitfalls remain. A common issue arises from low-quality images, which can significantly impact diagnostic accuracy. In this study, low-quality MEUS images were excluded, ensuring that only clear and focus-qualified images were used for model training and validation. Facilitating a rigorous quality control process is vital to mitigate the risk of misinterpretations. Similarly, access to comprehensive pathology reports ensures accurate diagnosis; thus, establishing reliable data collection standards is critical.
Tools and Metrics in Practice
Tools used in the analysis of MEUS images include VGG Image Annotator for manual annotation and statistical software like SPSS for statistical analysis. Metrics like AUC, sensitivity, specificity, accuracy, positive predictive value (PPV), and negative predictive value (NPV) were crucial in evaluating model performance. These metrics assist clinicians in understanding the reliability of the AI system compared to traditional diagnostic methods.
Variations and Alternatives
While the interpretable deep learning model has proven advantageous, there are alternatives worth considering. For instance, certain hospitals may opt for traditional imaging techniques over AI-assisted methods due to cost or resource limitations. However, although traditional methods can yield quality information, they may lack the interpretation and scalability that AI provides. As healthcare continues to evolve, the shift towards integrating AI-based solutions becomes increasingly relevant, especially in fields requiring high diagnostic accuracy.
FAQ
What are gastrointestinal stromal tumors (GISTs)?
GISTs are tumors that arise from the interstitial cells of Cajal in the digestive tract. They are often found in the stomach or intestines and can be benign or malignant.
How does microprobe endoscopic ultrasonography (MEUS) work?
MEUS utilizes a miniature ultrasound probe inserted through the endoscope to obtain high-resolution images of lesions within the gastrointestinal tract, allowing for precise assessments.
What benefits does deep learning provide in medical diagnostics?
Deep learning enhances diagnostic accuracy by analyzing complex patterns in imaging data, providing interpretable results in real-time, and potentially improving patient outcomes.
How can biases in AI diagnostics be addressed?
Ensuring diverse training datasets, regular evaluation, and validation against clinical outcomes can help address biases and improve model reliability over time.