Unveiling the MS Mosaic Mobile Application: A Comprehensive Overview
Overview of Approach
The development of the MS Mosaic mobile application marked a significant advancement in addressing the challenges faced by individuals living with Multiple Sclerosis (MS). This initiative emerged from a collaborative effort spanning two years, involving a blend of software engineers, MS care providers, data scientists, and participants living with MS. Central to the app’s design were extensive user experience research studies conducted with MS patients, ensuring that the final product not only met technical standards but also catered uniquely to user needs.
The application was officially launched in the United States on September 29, 2017, and over the subsequent three years, it facilitated a large-scale, site-less prospective case-control study running until December 19, 2020. During this period, collected data was retrieved, de-identified, and organized into sliding subject-time instances, each representing a week of participant data. This weekly structure was crucial for the model development phase, where predictions were made about the future severity of specific symptoms.
The predictive models aimed to ascertain whether the median self-reported severity of one of five targeted symptoms would exceed a score of two (indicative of moderate disability) over a three-month window. Subject data was utilized to classify instances with a score above this threshold as ‘true,’ signifying the presence of clinically actionable symptoms in the coming months. Crucially, only the data from participants who regularly engaged with the app over a minimum of three months was employed—culminating in a sample size of 713 for analysis.
Participant Distribution and Model Training
Random selection methods were applied to divide the dataset into a development cohort (567 individuals) and a blind test cohort (146 individuals). This methodology, augmented by 5-fold cross-validation, ensured robust model training and validation. To ultimately pinpoint the most effective predictive model, three classical machine learning techniques were tested alongside two deep learning methods. Notably, this multifaceted approach paved the way for a comprehensive understanding of symptom prediction.
Characteristics of the Study Population
The adoption of the MS Mosaic app was impressive, with over 1804 participants enrolling in the study. However, only 713 users, accounting for 39.52% of downloads, engaged with the application long enough (over three months) to contribute valuable data. The variability in app engagement was substantial, with the mean usage duration exceeding a year.
An interesting observation arose during the study concerning participant engagement, which saw a marked decline in March 2020, coinciding with the onset of the COVID-19 pandemic. This period of reduced app utilization inevitably influenced the study’s averages. For those who participated, demographic data revealed a mean age of 46.27 years, with the majority characterized by various comorbidities, including vitamin D deficiency (51.04%) and hypertension (18.78%).
Diving deeper into the MS diagnoses, a predominance of relapsing-remitting MS was noted among the cohort, with 77.37% of participants falling into this category. The persistence of symptoms such as fatigue, weakness, and cognitive changes was evident, exemplifying the daily struggles faced by individuals with MS. Reports of relapses also highlighted the variability in individual experiences, underlining the need for personalized monitoring tools.
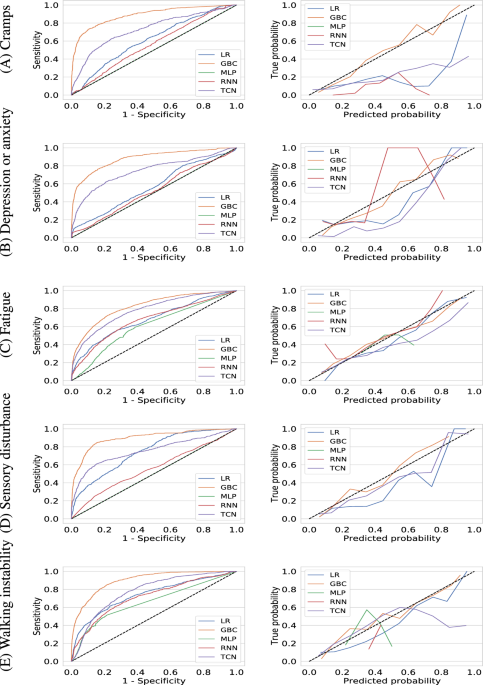
Model Discrimination and Performance Analysis
In evaluating the predictive efficacy of the models developed from the app’s data, key performance measures were documented. The results illustrated that the Gradient Boosting Classifier (GBC) consistently outperformed both classical machine learning methods and deep learning techniques in predicting high-severity symptoms across various domains. On the blind test cohort, for instance, GBC achieved a notable Area Under the Receiver Operating Characteristic Curve (AUROC) for symptoms like cramps and fatigue, demonstrating its clinical utility in real-world settings.
The consistency in performance was underscored by sensitivity and positive predictive value (PPV) metrics, which revealed a promising ability to accurately identify participants likely to experience symptom exacerbations, thus facilitating proactive clinical interventions.
Model Calibration
Aside from discriminative power, the ability of the predictive models to maintain calibration was equally imperative. Utilizing the Brier score for this purpose, it was found that GBC yielded the lowest scores across all symptoms, indicating that its predictions were not only accurate but also reliable with reduced uncertainty. Calibration curves further reinforced these findings, illuminating the model’s potential for real-time clinical application.
Subgroup Analyses: A Closer Look
Recognizing the diversity within the MS population, subgroup analyses were conducted based on MS subtypes and age demographics. Although the sample sizes for certain subgroups were small, the analyses generated insightful performance data. For instance, the GBC model exhibited superior outcomes for relapsing-remitting and secondary progressive subtypes compared to primary progressive MS, likely reflecting the varying complexities of these conditions.
Age-based comparisons also demonstrated a similar range of predictive efficacy across groups, reinforcing the notion that while age may play a role, the predictive power of the model is largely robust across different cohorts.
Identification and Importance of Predictive Features
An exciting aspect of this study centered on feature identification and the determination of which variables most significantly influenced symptom severity predictions. Various feature sets were compared, showcasing that symptom data distinctly accounted for the majority of predictive performance. This also highlighted that previous symptom trajectories were particularly informative, serving as a cornerstone for future symptom predictions.
Importantly, the study also employed feature ablation techniques, demonstrating how the exclusion of specific features affected model performance. The findings revealed a crucial relationship between past symptom data and future severity predictions, underscoring the need for comprehensive data integration in predictive modeling.
Feature Ablation Studies
Further investigations into the robustness of the models involved ablation studies and comparisons with baseline predictors. By removing critical features, it became evident how essential historical data was to maintaining high prediction accuracy. Interestingly, an alternative rule-based method showed significantly poorer performance, emphasizing the sophistication required in modern predictive algorithms.
In essence, these analyses enhance understanding not only of symptom prediction but also of the importance of leveraging comprehensive data to build effective healthcare tools.
Through the nuanced study of symptom trajectories, demographic factors, and predictive algorithms, the MS Mosaic application stands at the forefront of innovative health management solutions for individuals with MS. Its ability to predict symptom trajectories, empower users, and facilitate effective healthcare interventions showcases the transformative potential of technology in chronic disease management.