Understanding the Economic Impact of Spine Surgery
Spine surgery is a significant cornerstone of healthcare costs in the United States, comprising an estimated annual economic burden exceeding $24.3 billion. This figure isn’t just a statistic; it’s a reflection of the high volume and complexity associated with spinal procedures. As more patients turn to surgical options for relief from various spine-related conditions, the implications for healthcare economics escalate.
The Role of Bundled Payment Models
In an effort to manage these spiraling costs, the healthcare sector has seen the introduction of Value-Based Care (VBC) frameworks. Notable examples include Bundled Payments for Care Improvement (BPCI) and the advanced version, BPCI-A. These models aim to streamline costs by bundling payments for specific care episodes, incentivizing providers to deliver high-quality care efficiently. However, spine surgery has been slow to adopt these frameworks effectively, largely due to the nuanced nature of many spinal procedures.
Challenges in Implementation
One major hurdle is that existing Bundled Payment Models (BPMs) often rely on Major Diagnostic Categories (MS-DRGs), which can have substantial intra-coding variability. The heterogeneity of spinal surgeries—from single-level fusions to complex multi-level procedures—complicates risk adjustment, ultimately leading to suboptimal outcomes. Current BPMs have shown limited adaptability in addressing diverse patient demographics, comorbidities, and the inherently individualized nature of spine surgeries. Thus, overcoming these barriers requires predictive models capable of capturing the complexities inherent in spinal procedures and patient-specific factors.
Advancements in Risk-Stratified Payment Models
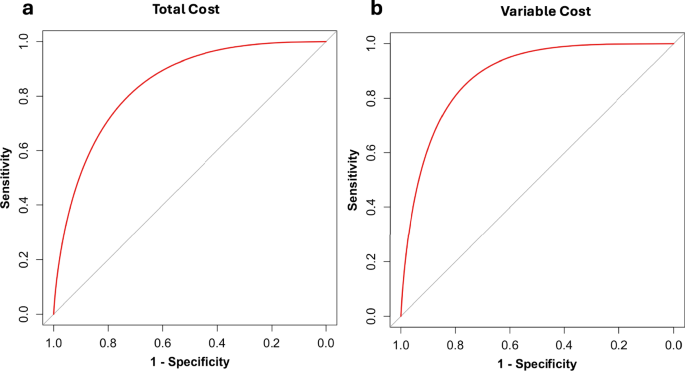
Our latest research proposes a multimodal Machine Learning (ML) framework designed to enhance risk-adjustment in spine surgeries. This new Patient-Specific Payment Model (PSPM) provides excellent predictive capabilities for outlier costs by accounting for various patient-centric factors. In fact, patients can fall into tiers ranging from a low-risk payment of around $17,682 to a high-risk payment exceeding $123,909. Notably, outlier patients—about 11% of our cohort—experienced severe complications, longer hospital stays, and a higher likelihood of reoperations, illustrating the limitations of the existing flat-rate, two-sided risk BPMs.
Financial Implications for Healthcare Providers
For providers, the financial ramifications of managing high-risk patients under flat-rate bundles can be daunting. Many surgeons have reported that their decision-making has shifted under bundled payment plans, impacting their willingness to take on complex cases. A refined BPM that incorporates patient-level risk could thus incentivize healthcare professionals to perform necessary surgeries without the looming fear of financial repercussions.
The Importance of Patient-Level Data
Interestingly, previous studies have emphasized that understanding patient-level data is crucial. Factors influencing surgical success go beyond mere financial considerations; the complexity of patient backgrounds, surgical approaches, and comorbid conditions must play a role in BPM design. Our PSPM aligns well with these perspectives, as it incorporates granular patient data to facilitate equitable and sustainable reimbursement strategies.
Comparative Effectiveness of Different Procedures
Economic evaluations reveal that not all spinal surgeries are created equal. For instance, cervical procedures like Anterior Cervical Discectomy and Fusion (ACDF) demonstrate a favorable cost-to-profit ratio, while lumbar procedures such as Transforaminal Lumbar Interbody Fusion (TLIF) show higher costs with lower profitability. This discrepancy emphasizes the need for financial strategies that effectively manage the complexities and risks associated with high-cost lumbar surgeries.
Diverse Patient Populations
Our study addresses a significant gap in existing research by focusing on a mixed-income, racially diverse patient population. Including data on social determinants of health (SDOH), like race, ethnicity, and insurance type, enhances the model’s applicability and underscores its potential to serve a wider array of patients who have historically been underrepresented in surgical outcome studies.
Enhancing Model Transparency
A noteworthy feature of our ML model is its transparency. Traditional AI models are often seen as "black boxes," making it challenging for clinicians to trust their outputs. Our approach seeks to mitigate this concern by identifying clinically understandable factors, such as preoperative hemoglobin levels and body mass index (BMI), that significantly influence predicted costs. By aligning model predictions with real-world clinical reasoning, we enhance trust between providers and the technology.
The Future of Predictive Healthcare Models
In forthcoming work, we aim to address current limitations, such as the absence of specific surgical data and the need for external model validation. Our objective is to create a flexible model that not only predicts costs but adapts to varying regional practices and patient demographics. Implementing these advancements will facilitate the development of a more comprehensive and user-friendly model for predicting costs in spine surgery.
Conclusion
Spine surgery exemplifies the complexities of healthcare economics. With ongoing innovations in predictive modeling and risk adjustment, the potential exists to improve patient outcomes while simultaneously managing costs effectively. By focusing on patient-specific factors and integrating advanced technological solutions, we may witness a shift towards more equitable and impactful healthcare practices in the field of spine surgery.