Understanding Keratoconus: Insights into a Complex Condition
Keratoconus is a condition that affects the cornea, a critical component of the eye’s optical system. The cornea serves as the eye’s outermost lens, responsible for focusing light onto the retina. In keratoconus, this once-clear and smooth structure begins to degenerate, leading to significant visual impairment. Typically diagnosed in the second or third decade of life, keratoconus manifests as a progressive, bilateral, and often asymmetrical condition characterized by corneal thinning and protrusion.
The Mechanism Behind Keratoconus
At the heart of keratoconus is collagen instability within the cornea. The cohesiveness of collagen fibers is essential for maintaining corneal structure and integrity. In keratoconus, there’s a disruption in these fibers, leading to biomechanical weakness. This progressive condition results in increased corneal curvature, often leading to irregular astigmatism and various refractive errors that cannot be corrected with traditional glasses.
Influencing Factors
Several factors contribute to the onset and progression of keratoconus. Recent studies suggest an inflammatory component, often linked to allergic or atopic conditions. Moreover, a positive family history indicates a genetic predisposition, although environmental influences, such as chronic eye rubbing—which is often a response to itching—can exacerbate the mechanical stress on corneal tissue.
Visual Impairment and Disease Progression
As keratoconus advances, the central or paracentral areas of the cornea exhibit significant thinning and steepening. This distortion results in high-order aberrations and irregular astigmatism, severely affecting visual quality. The progression of the disease is asymmetrical and can continue until well into a person’s 30s. An expansive meta-analysis encompassing over 50 million individuals across 15 countries estimated a global prevalence of keratoconus at approximately 138 cases per 100,000 people, with certain populations showing rates as high as 4.79%.
Diagnosis and Diagnostic Tools
Diagnosing keratoconus involves a multifaceted approach incorporating clinical evaluation and advanced imaging techniques. Medical history, visual acuity tests, and comprehensive slit-lamp examinations contribute to the diagnostic process. However, it’s the advanced imaging methods that have revolutionized the early detection of keratoconus.
Corneal topography and anterior segment optical coherence tomography (OCT) stand out as vital tools. Corneal topography provides a detailed map of the cornea’s surface, allowing clinicians to assess shape abnormalities, while OCT offers high-resolution, cross-sectional images of the cornea, facilitating the identification of subtle changes long before traditional examination techniques would.
Biomechanics in Diagnosis
Recent advances in measuring corneal biomechanics also offer valuable insights for diagnosis. Techniques like dynamic Scheimpflug imaging can accurately assess corneal stiffness and integrity, serving as essential markers for early disease detection. Engaging these advanced technologies enhances the ability to diagnose keratoconus and monitor its progression effectively.
Therapeutic Interventions
Once diagnosed, the goal is to manage keratoconus effectively and alleviate visual impairment. Corneal collagen cross-linking has emerged as a pivotal treatment, as it strengthens the corneal tissue and halts disease progression. Unfortunately, late-stage diagnosis often limits treatment options, with corneal transplant surgery becoming necessary when scarring or severe thinning occurs.
Access to appropriate diagnostic tools and timely interventions remains a challenge, particularly in low-resource settings. The scarcity of corneal donor tissue can lead to extensive waiting times for much-needed surgical procedures.
Technological Innovations in Early Detection
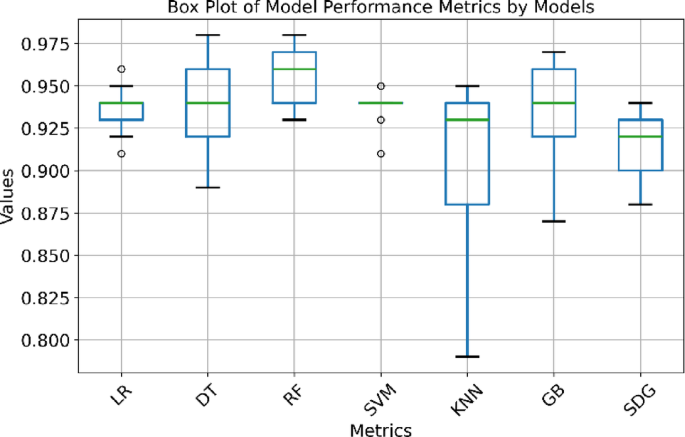
With ongoing advancements in technology, there’s growing enthusiasm about the role of machine learning in the diagnostic landscape of keratoconus. Algorithms that harness data from diverse imaging modalities, including spectral-domain OCT, Scheimpflug imaging, and tonometry, show promise for improving early detection and effectively classifying keratoconus severity.
Recent systematic reviews highlight how these algorithms have revolutionized early-stage detection, particularly for form fruste keratoconus (FFKC)—a subtle, early manifestation of the disease that can often go overlooked.
Emerging Technologies
Cutting-edge methodologies such as high-resolution ultrasound pachymetry and anterior segment OCT are also being explored, offering enhanced detail regarding corneal layers and epithelial thickness. These techniques boast a high specificity for identifying preclinical keratoconus.
Despite these developments, the diagnostic challenge remains in distinguishing the subtle signs of early disease from normal physiological variations. Continuous research aims to refine our understanding and enhance diagnostic accuracy through standardized machine learning models.
The Future of Keratoconus Management
The aim of future research is not just to enhance early diagnostic methods but to ensure these advancements are closely aligned with clinical practices. By integrating machine learning algorithms with structured data from comprehensive tests, medical professionals can distinguish healthy corneas from those affected by keratoconus more effectively.
In conclusion, the understanding and management of keratoconus is continuously evolving, driven by advancements in technology and growing knowledge of the disease etiology. Ongoing studies are crucial for refining diagnostic measures and treatment options, especially in the quest to maintain vision and improve quality of life for those affected by this condition.