Understanding Oral Potentially Malignant Disorders (OPMDs) and AI-Assisted Detection
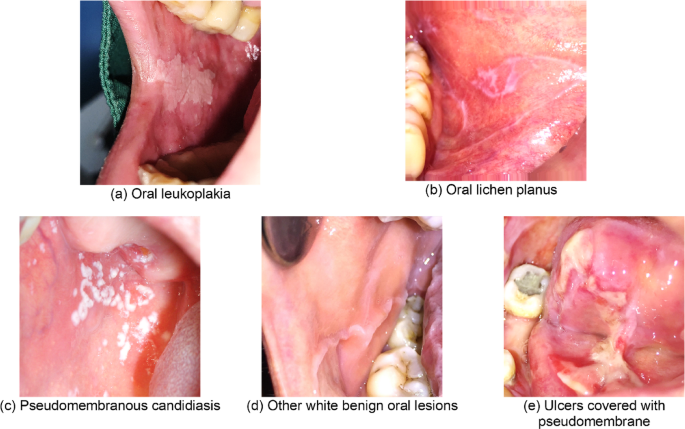
Oral Potentially Malignant Disorders (OPMDs) represent a significant concern in dentistry due to their potential to progress to oral cancer. Among OPMDs, conditions like leukoplakia and Oral Lichenoid Lesions (OLP) have a higher risk of malignant transformation compared to benign conditions like pseudomembranous candidiasis and ulcers. The accurate classification and diagnosis of these lesions are critical for timely interventions and improving patient survival rates.
The Risk Landscape of OPMDs
Leukoplakia and OLP are known for their cancerous potential, necessitating vigilant monitoring. Treatments and diagnostic protocols require a nuanced understanding of these conditions since early detection can significantly influence patient outcomes. On the other end of the spectrum, manageable conditions like candidiasis carry a very low risk of transitioning into cancer. Thus, effective diagnosis ensures appropriate referrals to specialists and mitigates unnecessary anxiety for patients.
Advances in AI for Diagnostic Classification
In recent years, deep learning models—specifically Convolutional Neural Networks (CNNs) and transformer architectures—have emerged as transformative tools in medical imaging. Researchers have explored various models to classify oral lesions regarding their malignancy risk. Notably, the IFormerBase transformer model demonstrated remarkable accuracy, achieving an accuracy rate of 0.86, with strong precision and F1 scores. On its heels was the DaViT_T transformer model, which also showcased promising results.
Performance Metrics of AI Models
The performance of these models is not just about high accuracy; it includes other crucial metrics such as precision (the correctness of positive predictions) and recall (the model’s ability to identify all relevant instances). Interestingly, the IFormerBase model displayed some misclassification issues, particularly with leukoplakia. Six OLP instances and other benign lesions were incorrectly categorized as leukoplakia, hinting at the complexities involved in distinguishing these conditions. However, this misclassification might not substantially impact the clinical workflow since both leukoplakia and OLP require further diagnostic scrutiny.
Misclassification and its Clinical Implications
Misclassifying benign lesions as potentially malignant adds undue pressure on clinical resources. While it’s essential to correctly identify conditions with a higher risk of cancer, it’s equally important to minimize unnecessary referrals that could burden specialists. Fortunately, the good recall rate for leukoplakia provides some confidence in leveraging these models for cancer screenings, despite the need for continual refinement.
Challenges in Multiclass Classification
The journey from multiclass to binary classification in machine learning often presents challenges. Reports have shown that multiclass classification typically yields lower performance metrics than binary tasks, emphasizing the need for specialized techniques tailored to complex situations in clinical settings. However, existing models, like DenseNet121, have reached impressive performance levels in distinguishing conditions like Oral Squamous Cell Carcinoma (OSCC) and healthy mucosa.
The Role of YOLO Architecture in Early Detection
In the realm of object detection, YOLO (You Only Look Once) models have gained traction for their speed and accuracy. A recent study confirmed the efficacy of YOLOv7 in classifying oral lesions into benign, potentially malignant, and malignant categories, delivering promising precision scores. Specifically, the YOLOv7-E6 model excelled in recognizing malignant lesions, indicating its potential for practical applications in clinical environments.
Analysis of YOLOv7 Performance
The performance metrics of YOLOv7, especially concerning OPMDs like leukoplakia and OLP, showed noteworthy outcomes. The model achieved impressive mean Average Precision (mAP) scores, reinforcing its reliability as a diagnostic tool. Understanding the visual characteristics of these lesions is beneficial; for instance, leukoplakia often presents as an elevated white plaque, serving as a marker for potential malignancy.
The Unseen Dataset Testing
Crucially, real-world applicability necessitates testing models on unseen datasets, ensuring they can generalize well beyond the training environments. YOLOv7 demonstrated robust performance across unseen test sets, outshining later versions of the YOLO architecture. This sets a high benchmark for future advancements, although it’s important to approach newer versions cautiously to ensure they meet or exceed established performance levels.
Insights on Limitations and Future Directions
However, limitations persist in the study of automated lesion identification, especially when reliant on a single dataset collected from specific institutions. Expanding the range of datasets and incorporating diverse image sources are essential next steps to enhance the models’ robustness and applicability.
Interpretable AI, particularly through techniques that visualize decision-making processes within models, will be critical for building trust in AI-driven solutions. Employing strategies like heat maps can help clinicians better understand the rationale behind model predictions, which is vital for effective clinical collaboration.
Efficiency in Model Training
Interestingly, the training duration for models like YOLOv7, clocking in at about 14.5 hours, illustrates the feasibility of integrating updated datasets. This operational efficiency is encouraging for clinical practice, posing AI-assisted diagnosis as a practical enhancement to traditional methods.
In conclusion, the intersection of dental healthcare and artificial intelligence offers promising avenues for early diagnosis and improved patient outcomes in managing OPMDs. With ongoing improvements and expansiveness in datasets, AI continues to emerge as a vital ally in the fight against oral cancers, ensuring clinicians are well-equipped to respond to and monitor these potentially malignant conditions effectively.