Understanding the Role of Deep Learning in Detecting Microsatellite Instability-High in Colorectal Cancer
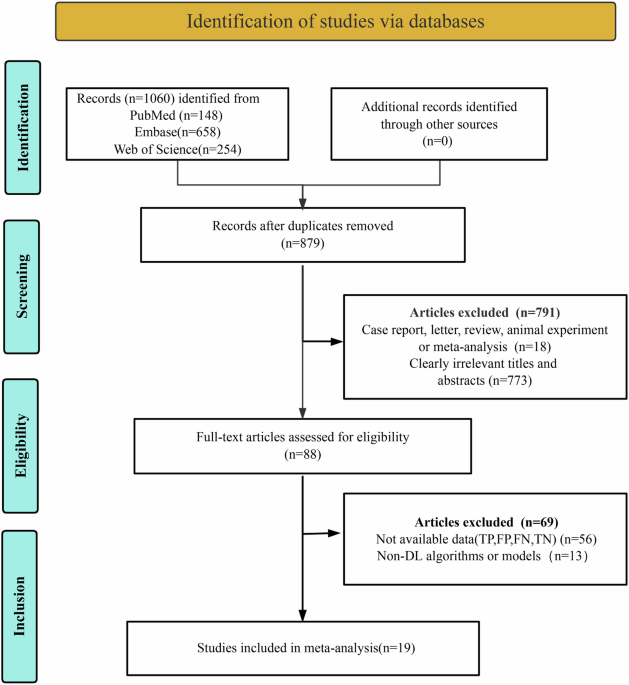
In recent years, the integration of deep learning (DL) algorithms into pathology has taken significant strides, particularly in the diagnosis of colorectal cancer (CRC). This article discusses a groundbreaking meta-analysis that delves into the diagnostic performance of DL algorithms for detecting microsatellite instability-high (MSI-H) in CRC using whole slide images (WSIs).
Key Findings from the Meta-Analysis
The meta-analysis presents some impressive statistics that highlight the effectiveness of DL in identifying MSI-H cases. In internal validation datasets, a patient-based approach recorded a sensitivity of 0.88 and specificity of 0.86. Meanwhile, an image-based analysis tracked slightly reduced values, with a sensitivity of 0.81 and specificity of 0.82. The area under the curve (AUC) for sensitivity stood at 0.94, while specificity documented 0.84.
In the external validation dataset, there was a noticeable leap in sensitivity to 0.93, though specificity was comparatively lower at 0.71. The corresponding image-based analysis yielded a sensitivity of 0.80 and specificity of 0.54. Here, the AUC reflected similar trends, with figures of 0.92 for patient-based analysis and 0.71 for image-based analysis.
The Power of DL Algorithms
So, what makes DL algorithms particularly effective in detecting MSI-H? A considerable advantage lies in their capacity to automatically learn intricate morphological features linked to MSI-H directly from digital pathology slides. This ability allows them to recognize aspects of pathology that may elude the trained eye of conventional pathologists.
The superior results observed in internal validation datasets can be attributed to consistent data preprocessing, uniform staining, and standardized image acquisition protocols. These elements help create a conducive environment for the model to differentiate MSI-H from non-MSI-H cases with higher accuracy.
In contrast, external validation datasets often present a multitude of variables. Differences in staining methods, slide preparation, and image quality result in significant challenges, leading to lowered specificity. Such discrepancies underscore the necessity for standardized data handling and multi-center datasets to enhance the generalizability of DL models.
Patient-Based vs. Image-Based Analysis
A particularly notable aspect of the analysis was the comparison between patient-based and image-based approaches. Patient-based strategies achieved higher sensitivity than their image-based counterparts, indicating a more robust analysis of the patients’ variability in tumor types and stages. Each patient was represented by a single WSI image, which captured a wider range of morphological variability compared to the multiple slices that image-based methods often employed.
Notably, relying on a patient-based approach not only leads to better adaptability across diverse populations but also allows the model to learn a broader spectrum of features encompassing tumor staging and demographic variables.
Meta-Regression Analysis Insights
The meta-regression analysis offered further insights into the performance of various DL algorithms, revealing no significant statistical differences in sensitivity and specificity between patient-based CNN and non-CNN groups. Different studies, such as that by Niehues, demonstrated the potential of self-supervised models to efficiently concentrate on relevant tissue regions, thereby maximizing predictive accuracy.
Interestingly, the size of the analyzed tiles played a pivotal role in diagnostic outcomes. Larger tiles (512×512) showcased a higher specificity than smaller ones (224×224 or 256×256), which might miss more localized pathological changes. This finding highlights the intricate balance required in designing input datasets for DL algorithms.
Reference Standards: PCR vs. IHC
An intriguing aspect of the analysis emerged when examining reference standards for identifying MSI in CRC. The results indicated that comparing the sensitivity between the non-only PCR group and the only PCR group demonstrated that the former had significantly greater sensitivity. Current evidence showcases that PCR provides a superior diagnostic performance as opposed to immunohistochemistry (IHC), particularly in terms of sensitivity and specificity.
Using IHC as the gold standard may inadvertently inflate false-positive rates, as it can wrongly classify non-MSI-H cases as positives. On the flip side, when PCR is used as the reference standard, the model requires more stringent accuracy, resulting in a clearer depiction of biological states.
Addressing Challenges and Limitations
Despite the compelling evidence supporting the utility of DL in MSI-H detection, challenges remain. Several studies included in the meta-analysis were retrospective, and the reliance on specific open datasets may limit the model’s generalizability. Additionally, issues such as data privacy, model interpretability, and regulatory approval further complicate the implementation.
With the landscape heavily characterized by heterogeneity, multiple factors like tumor staging, dataset size, and specimen origin can influence the observed results. The lack of prospective studies indicates a pressing need for future investigations to validate these findings more comprehensively.
Comparative Performance Against Human Pathologists
Only one study within the scope of the analyzed articles directly compared DL algorithms with human pathologist performance. This gap signifies a valuable avenue for further exploration, as understanding how DL models stack against seasoned pathologists can pave the way for integrating AI more effectively into clinical settings.
Economic Implications and Future Directions
Besides diagnostic performance, the economic implications of adopting AI models are promising. The potential to save healthcare costs while maintaining high accuracy suggests a win-win scenario for both patients and healthcare systems. Leveraging AI not only facilitates faster diagnosis but also allows for more informed treatment decisions, ultimately improving patient outcomes.
In light of ongoing research, the focus should pivot towards bolstering dataset sizes and diversity, thereby enhancing model robustness. Addressing the myriad challenges that accompany the deployment of AI in clinical practice remains essential in establishing a reliable and safe diagnostic framework. The journey toward a future where AI and pathology coexist in harmony is underway, with exciting prospects on the horizon.