Understanding Post-Stroke Depression: Insights and Innovations
The Significance of Post-Stroke Depression
Post-stroke depression (PSD) is a prevalent and debilitating condition that emerges in many stroke survivors. It affects not only quality of life but also the recovery process, complicating rehabilitation efforts. Studies indicate that the incidence of depression following a stroke varies, but estimates suggest it affects up to one-third of stroke patients. This staggering statistic highlights the importance of understanding the underlying causes and devising effective treatments.
Risk Factors and Predictive Models
Research has shed light on various predictors of PSD. Luo et al. (2023) developed a nomogram model that identifies individuals at high risk for developing post-stroke depression by analyzing clinical characteristics and genetic factors. These predictive models are pivotal as they enable healthcare professionals to implement early interventions, potentially improving patient outcomes.
The World Health Organization (WHO) has consistently reported on the burden of stroke and its complications, emphasizing the need for tailored mental health assessments post-stroke. As Ayerbe et al. (2013) pointed out in their meta-analysis, understanding the natural history and outcomes of depression after stroke can lead to more comprehensive care.
Biological and Neuroanatomical Insights
The pathophysiology of PSD is a complex interplay between biological, psychological, and environmental factors. Frank et al. (2022) reviewed current drug treatments for PSD, highlighting how the brain’s changes post-stroke — especially in regions associated with mood regulation — contribute to the onset of depression. In particular, lesions in the frontal lobe and basal ganglia have been implicated in depressive symptoms.
Recent studies have also linked inflammation and neurochemical imbalances with depression. Research by Chen et al. (2023) suggests that serotonin metabolism is disrupted in individuals suffering from post-stroke depression, revealing potential targets for therapeutic interventions. Understanding these underlying mechanisms is crucial for developing effective treatments and preventative strategies.
Current Treatment Strategies
Treatment for post-stroke depression often involves a multidisciplinary approach. Utilizing pharmacological options, such as antidepressants, alongside psychotherapeutic interventions has been at the forefront of managing PSD. Castilla-Guerra et al. (2020) evaluated pharmacological management techniques, indicating that personalized treatment plans can enhance recovery and improve overall quality of life.
In addition to medication, psychological counseling and rehabilitative strategies play vital roles. Cognitive-behavioral therapy (CBT) and mindfulness practices have shown promise in alleviating depressive symptoms among stroke survivors. VanDerwerker et al. (2018) examined the combined use of repetitive transcranial magnetic stimulation (rTMS) and aerobic exercises, showcasing a holistic approach that may yield beneficial results.
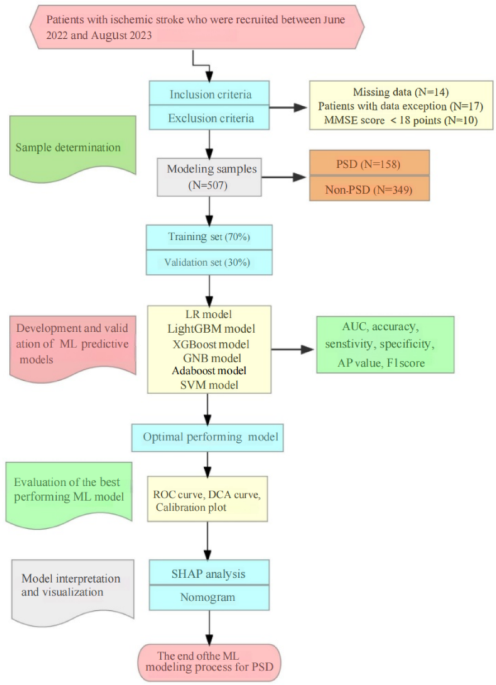
The Role of Machine Learning in Predicting PSD
Machine learning has emerged as a transformative tool in predicting and managing post-stroke depression. Algorithms can analyze vast amounts of data, identifying patterns and risk factors that may not be immediately evident through traditional clinical assessments. Chen et al. (2023) explored a machine learning algorithm that utilized real-world data to forecast new-onset PSD, emphasizing how technology can enhance predictive accuracy and early detection.
Moreover, advancements in artificial intelligence can assist in personalizing patient care by tailoring interventions based on individual risk profiles. This technological integration is a promising frontier in improving mental health outcomes post-stroke.
The Impact of Lifestyle Factors
Lifestyle factors significantly influence the trajectory of post-stroke recovery and the risk of depression. Sleep quality, nutrition, and physical activity are crucial elements that can either mitigate or exacerbate depressive symptoms. Studies have reported that stroke survivors experience sleep disturbances, which can lead to enhanced fatigue and depressive symptoms.
Research by He and Ruan (2022) underscores the association between poor sleep quality and the onset of depression among stroke patients. Additionally, nutrition plays a fundamental role in mental health; diets rich in omega-3 fatty acids and vitamins have been linked to improved mood and cognitive functioning.
Future Directions in Research
Ongoing research aims to deepen our understanding of post-stroke depression and enhance therapeutic strategies. The development of newer predictive models, as seen in the works of Gong et al. (2023) and Liu et al. (2023), promises to advance clinical practices and patient care methodologies. Innovations in neuroimaging techniques and biomarker studies further pave the way for a more nuanced understanding of how post-stroke depression manifests and can be effectively treated.
Collectively, these insights highlight the intricate relationship between stroke recovery and mental health, emphasizing the need for integrated care approaches that address both physical and psychological well-being. Ensuring comprehensive assessments and interventions can lead to better outcomes for stroke survivors grappling with the shadows of depression.