Detecting Hidden Movements in Patients with Acute Brain Injury Using SeeMe
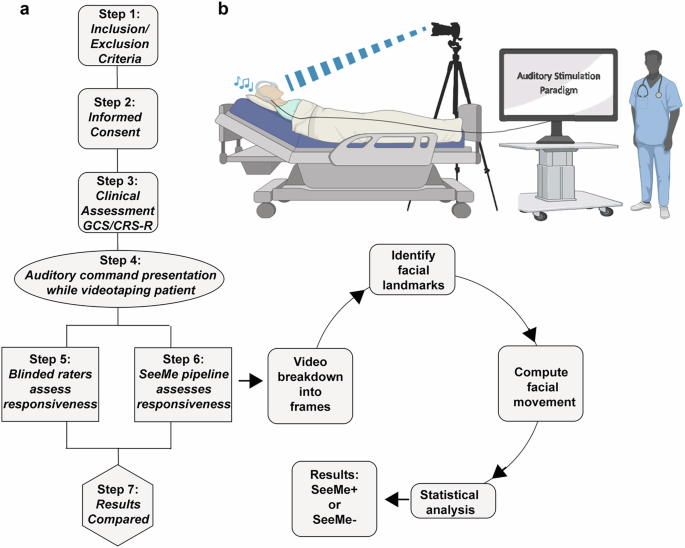
In recent research, a groundbreaking method called SeeMe was employed to observe subtle movements in patients with Acute Brain Injury (ABI), movements that are often imperceptible to the naked eye. This innovation might reshape how clinicians assess recovery and responsiveness in patients who are comatose or appear unresponsive.
Study Overview
The study featured 37 ABI patients along with 16 healthy control subjects. Researchers recorded a total of 872 videos that captured auditory stimulation, encompassing over 8,500 individual commands. Upon analyzing these recordings, they identified 423 videos as suitable for scrutiny—specifically, 92 videos focused on the command “Stick out your tongue,” 246 on “Open your eyes,” and 85 on “Show me a smile.”
Out of the ABI cohort, 36 patients produced analyzable videos for the eye command, while 17 patients did so for the mouth commands. Impressively, responses to the “Open your eyes” command were identified in 30 of the 36 patients, and responses to mouth commands were detected in 16 of 17. The findings are illustrated in various figures and heatmaps, showcasing positive movements detected by SeeMe, which were marked distinctly from those identified by blinded raters.
Sensitivity of SeeMe vs. Blinded Raters
Two blinded raters were tasked with evaluating the videos for stimulus-evoked movements. On average, they identified only 2.8 trials as responsive to the command, whereas SeeMe recognized an average of 5.4 responsive trials per session. This dramatic difference showcases SeeMe’s heightened sensitivity to low-amplitude movements. Such robust results raise questions about the reliability of traditional assessments in ABI settings and endorse the use of advanced detection technologies.
Exemplary Case Studies
Among the participants, Subject 13 was an older adult involved in a severe motor vehicle accident. Initial CT scans revealed multiple serious injuries, and he was in a deep coma upon admission. Remarkably, SeeMe detected stimulus-evoked movements as early as 18 days post-injury. His recovery demonstrated significant progress, evidenced by improvements in his Glasgow Coma Scale (GCS) score and eventual ability to follow commands.
Another case study, Subject 2, a middle-aged cyclist, displayed similar trends. After sustaining critical head injuries, his eye opening was confirmed by SeeMe before clinical assessments. This aligns symptomatically with the findings that SeeMe consistently detected vegetative or minimally conscious states earlier than traditional methods.
SeeMe’s Early Detection of Consciousness
The data revealed a critical insight: SeeMe was able to detect movements before they were observed by clinicians in many cases. Specifically, it identified eye or mouth movements in 30 out of 36 patients prior to clinical detection in 16 of those cases. This places SeeMe in a revolutionary position regarding how medical professionals might assess patient recovery trajectories.
For example, on average, SeeMe detected eye-opening at approximately 9.1 days post-injury, while clinical examinations did so around 13.2 days post-injury. This revelation suggests that SeeMe has the potential to advance our understanding of consciousness recovery significantly.
Correlating SeeMe Outcomes with Functional Recovery
As patients progressed in their recovery, the amplitude of their movements also increased, establishing a distinctive link between SeeMe’s findings and positive patient outcomes. Researchers explored how well SeeMe’s performance corresponded to discharge outcomes measured by the Glasgow Outcome Scale—Extended (GOS-E). The results indicated a strong positive correlation between movement amplitude and frequency with more favorable recovery outcomes.
Validating Results with Classifiers
To address doubts regarding the interpretation of movements, researchers developed a deep neural network aimed at differentiating commands based on the facial movements detected. The classifier achieved a solid rate of 65% overall accuracy, affirming that SeeMe not only identifies movements but is also capable of understanding their context.
Implications for Clinical Practice
The findings from the SeeMe assessments provide a transformative perspective on how we might evaluate consciousness and responsiveness in ABI patients. By integrating advanced technologies like SeeMe into clinical practice, healthcare providers may enhance their diagnostic processes and ultimately improve patient outcomes.
Through this innovative research, SeeMe stands as a promising addition to the toolkit of medical professionals working with ABI patients, paving the way for more nuanced understanding and earlier detection of changes in consciousness.