Harnessing Natural Language Processing in Prostate Cancer Consultations
Introduction to NLP in Healthcare
Natural Language Processing (NLP) is transforming the way healthcare professionals analyze and interpret patient interactions. In prostate cancer consultations, where nuanced communication is vital for shared decision-making (SDM), NLP tools can enhance understanding and clarity. A recent study meticulously crafted an NLP model using a comprehensive dataset derived from 50 patient consultations led by 10 multidisciplinary providers.
Composition of the Development Dataset
The development dataset consisted of 28,927 sentences extracted from the consultations, illustrating diverse patient-provider dialogues. To ensure robust training and validation, 75% (21,695 sentences) of the dataset was designated for model training, while 25% (7,232 sentences) was reserved for internal validation purposes. This methodical partitioning helps prevent overfitting and ensures the model’s generalizability.
Key Concepts and Their Representation
Among the total sentences, several key concepts were identified and manually coded, including:
- Tumor Risk (TR): 356 sentences (1.2%)
- Pathology Results (PR): 707 sentences (2.4%)
- Life Expectancy (LE): 126 sentences (0.4%)
- Cancer Prognosis (CP): 333 sentences (1.2%)
- Urinary Function (UF): 94 sentences (0.3%)
- Erectile Function (EF): 81 sentences (0.3%)
- Erectile Dysfunction (ED): 600 sentences (2.1%)
- Urinary Incontinence (UI): 350 sentences (1.2%)
- Lower Urinary Tract Symptoms (LUTS): 302 sentences (1.0%)
Each of these elements plays a crucial role in understanding patient concerns and aiding their decision-making processes.
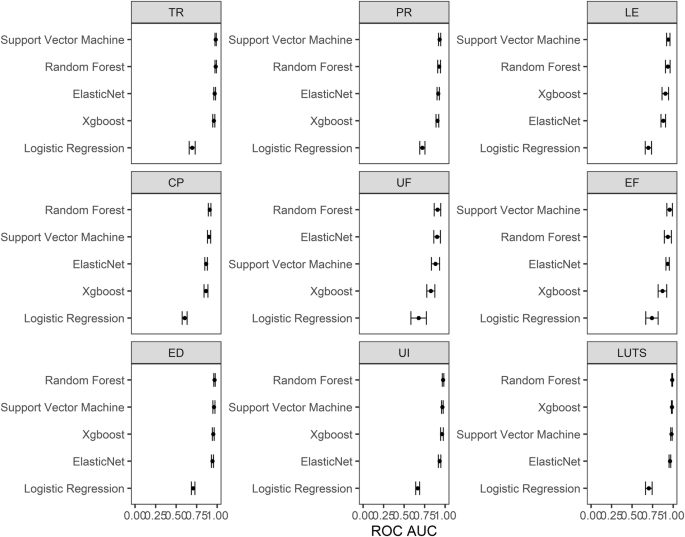
Efficacy of the Random Forest Model
Among various candidate models, the Random Forest model emerged as the most effective in predicting key concepts, achieving the highest Area Under the Curve (AUC) in Receiver Operating Characteristic (ROC) analysis across five key concepts. It also secured the second-highest AUC for the remaining four concepts, indicating a promising performance without significant statistical differences compared to the top-performing model. This robustness warranted the use of the Random Forest model in subsequent phases of internal validation and quality evaluation.
Internal Validation Processes
During internal validation, the Random Forest model maintained impressive AUC scores across the concepts:
- TR: 0.98 (95% CI 0.95–0.99)
- PR: 0.94 (95% CI 0.92–0.96)
- LE: 0.89 (95% CI 0.81–0.95)
- CP: 0.92 (95% CI 0.89–0.95)
- UF: 0.84 (95% CI 0.73–0.93)
- EF: 0.96 (95% CI 0.93–0.98)
- ED: 0.98 (95% CI 0.97–0.99)
- UI: 0.97 (95% CI 0.96–0.99)
- LUTS: 0.99 (95% CI 0.99–0.99)
These elevated AUC values indicate a strong predictive capacity, making the model a valuable asset in clinical environments.
Sensitivity and Specificity Metrics
The model’s sensitivity and specificity were also promising, ranging from 0.62 to 0.94 for sensitivity and 0.86 to 0.97 for specificity. This range illustrates the model’s ability to correctly identify relevant sentences linked to the various key concepts, vital for effective risk communication in prostate cancer consultations.
The Impact on Quality of Risk Communication
The analysis extended to a validation dataset comprising 9,367 sentences from 20 consultations, not included in previous training or validation phases. This dataset aimed to assess the quality of risk communication correlated with NLP-based predictions. Higher probabilities predicted by the model directly correlated with improved quality scores in risk communication.
In fact, among sentences quantifying risk, a striking 86% were captured at NLP probabilities exceeding 60%, with 76% at probabilities over 70% and 72% at greater than 75%. This demonstrates the model’s efficacy in capturing meaningful and quantifiable risk data essential for informed patient decision-making.
Determining Optimal Sentence Cutoffs
Exploring the number of model-derived sentences used in quality assessment revealed that limiting analysis to the top five sentences significantly lowered accuracy compared to using the top ten. Further refinement in the methodology indicated that analyzing 15 or 20 sentences yielded only minor improvements. Therefore, the optimal strategy was determined to be grading the top ten sentences with the highest topic concordance for an effective balance of accuracy and feasibility.
Accuracy and Feasibility of the Protocol
The resultant scoring protocol demonstrated exceptional accuracy in identifying relevant topics:
- TR: 100%
- PR: 90%
- LE: 95%
- CP: 95%
- UF: 80%
- EF: 95%
- ED: 85%
- UI: 100%
- LUTS: 95%
These results reflect a successful alignment with manual coding, reaffirming the model’s reliability in clinical settings and its potential to support healthcare providers in enhancing patient discussions.
Conclusion
The innovative application of the Random Forest model showcases how NLP can significantly improve the analysis of patient-provider interactions within prostate cancer contexts. By refining methods to ensure precision in data interpretation, healthcare professionals are better equipped to support patients through complex decision-making processes, ultimately leading to improved care outcomes.