“AI-Powered Deep Learning for Multi-Label X-Ray Screening of Knee Abnormalities: A Dual-Center Study”
AI-Powered Deep Learning for Multi-Label X-Ray Screening of Knee Abnormalities: A Dual-Center Study
Core Concept of AI in Medical Imaging
Artificial Intelligence (AI) has revolutionized the medical imaging field, particularly through deep learning models tailored for analyzing X-ray images. In this context, "deep learning" refers to a subset of machine learning techniques that use neural networks with several layers to process complex data patterns. This approach is crucial for improving the accuracy and efficiency of diagnosing multiple conditions from X-rays, leading to quicker interventions and better patient outcomes.
For example, consider a traditional X-ray analysis process where a radiologist views the image and identifies abnormalities manually. While effective, this approach can be time-consuming, and human error may occur. In contrast, an AI system can analyze thousands of images quickly, identifying abnormalities like meniscus tears or ligament injuries using pattern recognition. This transforms diagnostics, making it faster and more reliable.
Importance of Multi-Label Classification in Diagnosing Knee Abnormalities
Multi-label classification in medical imaging enables algorithms to identify several knee abnormalities simultaneously from a single X-ray image. This contrasts with single-label classification, where the model focuses on identifying just one condition. Given the complexity and interrelated nature of knee injuries, such as those involving the anterior cruciate ligament (ACL) and medial meniscus simultaneously, multi-label classification significantly enhances diagnostic accuracy.
For instance, a model trained to detect both ACL tears and joint effusion can offer more comprehensive insights from one single X-ray. This method addresses the clinical reality where knee injuries often coexist, improving both patient management and treatment outcomes.
Key Components for Successful AI Model Development
Several core components are essential for building an effective deep learning model for knee X-ray screening. These include data acquisition, preprocessing, model architecture selection, training, and evaluation metrics. Each component plays a critical role in the overall success of the AI application.
Data acquisition involves collecting high-quality X-ray images and corresponding diagnostic labels. In our study, X-ray images were sourced from two medical centers, ensuring diverse clinical data. Preprocessing, which includes normalization and resizing images, is crucial for maintaining consistency across datasets, thus aiding the model’s training phase.
For model architecture, selecting a well-established convolutional neural network (CNN) enhances feature extraction from images. In this study, networks like ResNet152 and DenseNet121 were utilized for their proven effectiveness in image analysis. Training the model using accurate datasets prepares it for reliable performance in real-world clinical settings.
Step-by-Step Process in the Study’s Implementation
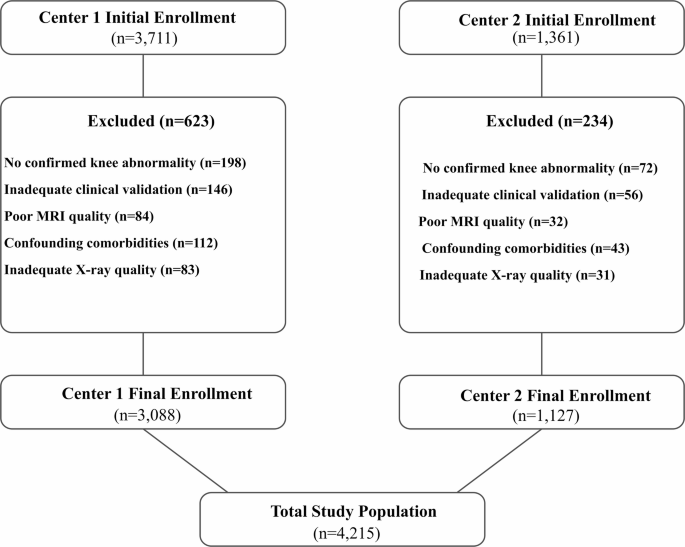
The study followed a systematic process, starting with patient recruitment and ending with model evaluation. Initially, adults undergoing knee X-ray imaging were enrolled based on specific criteria, such as age and clinical indications for imaging.
Next, a rigorous exclusion process ensured only relevant cases were included, particularly those confirming knee abnormalities. Following this, images were collected using a standardized protocol to guarantee consistency across scans, which is vital for AI analysis.
After image acquisition, deep learning models were trained on the labeled dataset. Hyperparameters were finely tuned, and multiple neural network architectures were tested to identify the one yielding the best performance in terms of detecting multiple abnormalities.
Practical Scenario: Using AI in Clinical Settings
The practical application of AI models for knee X-rays could transform emergency rooms or outpatient clinics where rapid assessments are necessary. For example, a patient presenting with knee swelling might undergo an X-ray. An AI system can analyze it in real-time, flagging various abnormalities such as ACL tears, joint effusion, or meniscal injuries.
This immediate feedback can assist physicians in quickly deciding whether to refer to a specialist for further evaluation or initiate treatment immediately. The ability to receive such insights in moments improves clinical workflows and patient satisfaction significantly.
Common Mistakes in AI Model Development and Solutions
Developing an AI model is fraught with potential pitfalls. A common mistake is overfitting, where a model performs well on training data but poorly on unseen data. This happens when a model becomes too complex. To solve this, techniques like data augmentation—introducing variations in the training dataset—can help ensure the model generalizes well to new data.
Another mistake is inadequate validation. If models are not tested on a sufficiently diverse dataset, their reliability can be questionable in clinical practice. Implementing robust validation leave-out methods increases confidence in model performance across different patient demographics.
Evaluation Tools and Metrics for the AI Models
A range of metrics was employed to assess model performance, including Mean Average Precision (mAP), Overall Precision (OP), and Overall Recall (OR). These metrics provide a comprehensive picture of how well the AI model predicts multiple conditions from a single X-ray.
For instance, mAP offers insights into how precisely the model identifies each abnormality, while OP and OR both reflect its effectiveness in correctly classifying true positive cases. By combining these metrics, a nuanced understanding of the model’s strengths and weaknesses can be achieved.
Alternatives to Multi-Label Classification
While multi-label classification is advantageous for detecting various conditions simultaneously, it does come with its own set of challenges, such as increased computational complexity and the need for extensive labeled data. Alternative approaches include single-label classification, which simplifies the model and training process but may miss concurrent abnormalities.
Models can also employ hierarchical classification, where the model first identifies broader categories before zooming in on specific conditions. The choice among these methodologies depends on clinical needs, available data, and desired outcomes—each offering unique pros and cons worthy of consideration.
Frequently Asked Questions
Q: How does the AI model handle overlapping injuries?
A: The model is designed to recognize multiple abnormalities simultaneously, ensuring it accounts for overlapping injuries like meniscus tears and ligament injuries found together.
Q: What is the significance of training on diverse datasets?
A: Training on diverse datasets increases the model’s ability to generalize, improving its reliability and effectiveness in real-world clinical settings.
Q: How long does it take for the AI model to analyze an X-ray image?
A: The analysis time can vary, but the goal is to achieve results within seconds to minutes, enabling quick decision-making for physicians.
Q: Are results from AI systems definitive in diagnosis?
A: While AI systems significantly enhance diagnostic accuracy, results should complement, not replace, clinical judgment.