Understanding Patient Demographics and Baseline Characteristics in Rheumatoid Arthritis Studies
In recent research involving the Bioreg dataset, a comprehensive investigation of patient demographics and baseline characteristics was conducted to assess remission in rheumatoid arthritis (RA) patients treated with biologic Disease-Modifying Anti-Rheumatic Drugs (bDMARDs). The journey of this study began with an impressive pool of 4,344 patients, eventually narrowing down to a final cohort of 1,223 patients who met specific criteria for inclusion. This journey reflects a meticulous approach to data analysis and highlights the significance of understanding patient characteristics for effective treatment outcomes.
Data Selection and Patient Cohort
Initially, the study aimed to gather data from 4,344 patients. However, after applying stringent inclusion criteria—focused on follow-up visits—only 1,494 patients remained. The subsequent requirement for a six-month follow-up DAS28-ESR score further narrowed the group: 271 patients were excluded for lack of this critical data. The final sample size—1,223 patients—ensured that the analysis would be both relevant and reliable, highlighting the importance of having robust data for predictive modeling.
Table 1 Overview
To lay a solid foundation for understanding intervention effectiveness, Table 1 summarizes the baseline characteristics of these 1,223 RA patients. The table includes key clinical features expressed as means, standard deviations, or percentages. Additionally, it draws a comparison between patients who achieved remission and those who did not, providing insight into what factors may influence treatment responses.
In parallel, 154 RA patients screened at the Erlangen site were included, providing an opportunity to examine these characteristics in a real-world setting—a crucial consideration when evaluating treatment efficacy.
Table 2 Overview
Table 2 delves deeper into the baseline clinical characteristics of these 154 RA patients specifically in Erlangen. This stratification allows researchers to identify trends within a more localized patient population, ensuring a thorough understanding of the clinical environment.
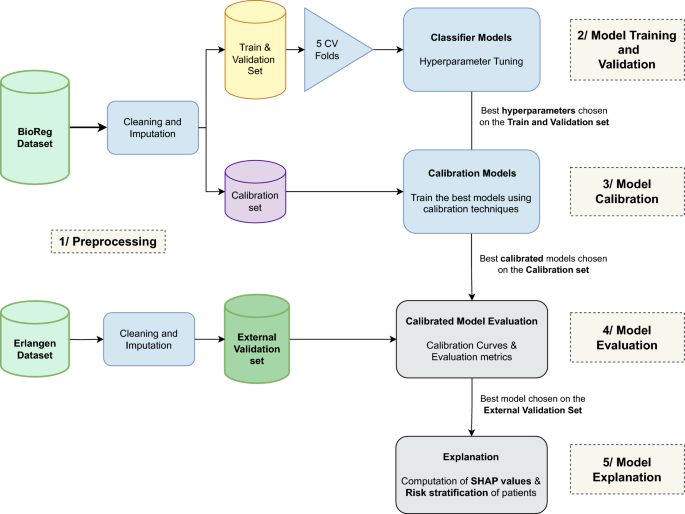
Predictive Modeling and Performance Metrics
With the backend data cleaned and patients categorized by remission status, the focus shifted towards predictive modeling. Several models—AdaBoost, Random Forest, Support Vector Machine (SVM), and XGBoost—were employed to identify patient remission outcomes after six months. Following hyperparameter tuning, these models underwent evaluation using a test set from the Erlangen dataset.
The performance metrics, summarized in Table 3, illustrate the varied effectiveness of each model in predicting remission. AdaBoost distinguished itself with consistent performance across numerous metrics. Despite XGBoost demonstrating the highest area under the receiver operating characteristic curve (AUC-ROC),the balanced approach from AdaBoost made it the most viable option for predicting remission effectively.
The Ensemble Methods Advantage
One of the standout findings was the strength of ensemble methods like AdaBoost and XGBoost. These models, by synthesizing predictions from multiple learners, displayed not only improved accuracy but also resilience to overfitting. Such capabilities are particularly handy when dealing with data variability, as seen in the Erlangen dataset.
Calibration and Model Reliability
To ensure the reliability of these models, a significant focus was also placed on calibration methods. Calibration curves were employed to measure the alignment between predicted probabilities and actual outcomes. Various techniques—including Platt scaling, isotonic regression, spline calibration, and beta calibration—were evaluated.
AdaBoost’s Calibration Performance
In the case of the AdaBoost model, the calibration curves indicated some over- and underestimations of predicted probabilities. Pre-calibration, the Brier score stood at 0.20, suggesting there was considerable room for improvement. Post-calibration, isotonic regression achieved a lower score of 0.13, demonstrating enhanced alignment between predicted and observed outcomes. This optimized prediction model served as an example of the importance of enhancing predictive accuracy through careful calibration.
SVM and Other Model Performances
The SVM model, while showing some initial promise, ultimately revealed shortcomings in calibration. The uncalibrated model’s pre-Brier score of 0.17 highlighted the need for refinement, but calibration methods offered only modest improvements. In contrast, the Random Forest and XGBoost models also showcased their calibration performances, demonstrating varying degrees of success based on the applied techniques.
Explainability through SHAP
An essential aspect of predictive modeling in healthcare involves not just predicting outcomes but also elucidating how those predictions are made. Utilizing SHapley Additive exPlanations (SHAP), the study illuminated which baseline features most influenced the predictions made by the AdaBoost classifier.
Feature Importance Insights
The results were telling: The DAS28 Score at baseline emerged as the most significant predictor, followed by the Visual Analog Scale (VAS) score, age, and swollen joint count (SJC). Higher values in these factors indicated lowered chances of remission. Such insights are invaluable for clinicians, guiding them to make more informed treatment decisions based on clinical indications.
Risk Stratification Outcomes
Leveraging the capabilities of the AdaBoost model, patients were stratified into three risk categories—low, medium, and high risk—based on their predicted probabilities of achieving remission. By offering clear gradations in treatment responses, these categories provide useful benchmarks for clinical practices.
Observed Remission Rates
The outcomes correlated strongly with the predicted risk levels. In the low-risk category, 89.7% of patients achieved remission, contrasting sharply with only 24.1% and 15.8% in the medium- and high-risk groups, respectively. This observed trend reaffirms the model’s utility in clinical decision-making based on predicted patient responses.
This refined exploration of patient demographics and baseline characteristics offers a window into the complexities of RA treatment and the use of predictive modeling to enhance clinical outcomes. By understanding the nuances of this data, healthcare practitioners can leverage these insights to tailor approaches for individual patients more accurately.