“Multimodal Deep Learning Model for Predicting Breast Cancer Recurrence Risk and Oncotype DX Correlation”
Multimodal Deep Learning Model for Predicting Breast Cancer Recurrence Risk and Oncotype DX Correlation
Core Concept of Multimodal Deep Learning in Breast Cancer
Multimodal deep learning (MDL) combines various data types to improve predictive accuracy in medical applications. In breast cancer, this approach leverages clinical data, imaging, and genomic information to assess recurrence risk more effectively than using a single modality. By integrating these diverse data sources, the model not only enhances prediction reliability but also tailors treatment strategies, potentially improving patient outcomes (Breast Cancer Research, 2025).
Key Components and Variables
Several critical components comprise the MDL model. First, clinical data includes patient demographics, tumor characteristics, and treatment history. For instance, age and menopausal status are collected, as they influence prognosis. Imaging data, particularly from MRI scans, is captured to analyze tumor features through different sequences like diffusion-weighted imaging (DWI) and dynamic contrast-enhanced MRI (DCE-MRI). Gene expression data from Oncotype DX tests further enrich the model, enabling assessments of tumor biology and risk stratification.
Even subtle differences in these variables can lead to significant disparities in treatment decisions. For example, a higher Oncotype DX recurrence score indicates a greater need for chemotherapy, impacting treatment approaches directly.
Step-by-Step Process of Model Development
Developing the MDL model follows a systematic lifecycle comprising:
-
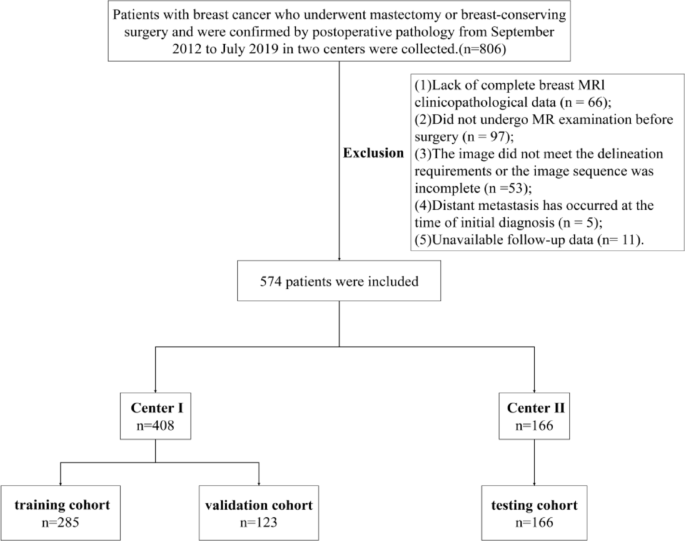
Patient Data Collection: Information is sourced from clinical records of patients diagnosed with non-metastatic invasive breast cancer. For example, the study included 622 patients, ultimately narrowing to 574 based on specific inclusion and exclusion criteria (Breast Cancer Research, 2025).
-
Image Acquisition and Preprocessing: MRI scans are conducted to visualize the tumor area. Image segmentation is performed using software like 3D Slicer, focusing on areas free from necrosis and other artifacts.
-
Data Integration: The model synthesizes imaging data and clinical variables alongside genomic data from the Oncotype DX test, which assesses gene expression related to cancer recurrence.
-
Feature Extraction: Advanced techniques extract significant radiomic features from the imaging data, such as geometric and textural attributes.
-
Model Training: A deep learning architecture, specifically ResNet18, is employed to classify recurrence risk using a combination of features from the MDL.
- Validation and Testing: The model undergoes rigorous testing using independent datasets, ensuring its robustness and predictive accuracy.
This structured approach emphasizes the importance of integrated data in enhancing predictive capabilities, ultimately guiding clinical decision-making.
Practical Examples of Model Implementation
In a practical application of this model, the implementation on a cohort of 574 breast cancer patients allowed for detailed analysis and prediction of recurrence risk. In one case, a patient’s clinical data indicated low recurrence risk based on conventional methods, yet the MDL model identified features suggesting increased risk. This can lead to an adjustment in treatment, demonstrating how multimodal approaches can uncover hidden risk factors.
Common Pitfalls and Solutions
One major pitfall in developing MDL models lies in data imbalance. For example, if most patients are classified as low-risk, the model may be biased toward that classification, reducing its overall effectiveness. To counter this, techniques like the Synthetic Minority Over-sampling Technique (SMOTE) can balance the dataset, ensuring that the model learns to identify both high and low-risk patients effectively.
Another issue can stem from overfitting the model to training data, which diminishes its predictive power on new examples. Incorporating techniques like cross-validation helps ensure that the model generalizes well to unseen data, enhancing clinical applicability.
Tools, Metrics, and Frameworks in Practice
Several tools and frameworks facilitate the development and implementation of MDL. The OnekeyAI platform, for instance, assists in data preparation and model training. Metrics such as receiver operating characteristic (ROC) curves evaluate model performance, allowing researchers to assess the trade-offs between sensitivity and specificity. Calibration metrics like the Hosmer–Lemeshow test further verify that predicted probabilities align closely with actual outcomes.
Moreover, statistical tools such as the R language aid in comprehensive data analysis and visualization, significantly enhancing interpretability and clinical utility.
Variations and Alternatives to MDL
While MDL shows promise in improving predictive accuracy, alternatives exist. Classical models based solely on radiomic features can help in scenarios with limited data availability or when genomic information is not accessible. However, these models often fall short in capturing the complexity of multifactorial influences. The trade-off here is a balance between data richness and necessity, with MDL offering a comprehensive approach when multifaceted data is available, while traditional methods provide efficiency in resource-constrained environments.
FAQ
What is the primary advantage of using multimodal deep learning in cancer prediction?
MDL integrates diverse data types, enhancing the depth and accuracy of predictions compared to single-source analyses.
How does the Oncotype DX test influence treatment decisions?
The Oncotype DX test scores help determine whether patients should receive chemotherapy based on their recurrence risk, significantly impacting treatment plans.
What strategies can prevent overfitting in deep learning models?
Incorporating techniques like cross-validation, limiting dataset size during training, and employing regularization methods can help prevent overfitting in models.
Can the MDL model be used in other types of cancer?
Yes, the principles of MDL can be adapted to predict outcomes and risks in various cancer types, given the necessary multimodal data.