“Predicting Obesity Risk with a Machine Learning Framework”
Predicting Obesity Risk with a Machine Learning Framework
Understanding Obesity Risk Prediction
Obesity risk prediction is the process of estimating an individual’s likelihood of becoming obese based on various data factors such as lifestyle, demographics, and health history. This area matters significantly as obesity is linked to multiple health conditions, including diabetes and cardiovascular diseases (WHO, 2022). Early identification can lead to timely interventions, ultimately reducing healthcare costs and improving individual health outcomes.
Key Components in Obesity Prediction
The framework for predicting obesity risk incorporates several key components including:
- Data Collection: Gathering extensive information on factors such as age, gender, weight, dietary habits, and physical activity.
- Feature Selection: Identifying which of these factors are most predictive of obesity using algorithms like the entropy controlled-quantum bat algorithm (EC-QBA).
- Machine Learning Algorithms: Employing various algorithms to analyze the selected features and predict obesity risk.
For example, the EC-QBA algorithm is notable for effectively selecting features by optimizing key parameters through both entropy and quantum mechanics. Such methodological rigor can lead to more accurate predictions and better understanding of obesity risk determinants.
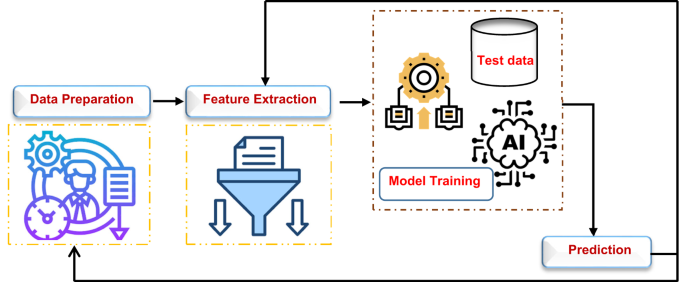
The Step-by-Step Process of the Framework
The lifecycle of the obesity risk prediction process consists of three main stages:
-
Preprocessing: This initial phase includes data cleansing practices such as filling missing values, normalizing the data, and removing outliers. Proper preprocessing enhances data quality, which is crucial for effective modeling.
-
Feature Selection: Using EC-QBA, the most relevant features are selected based on their predictive power. This step ensures that the model focuses on significant variables like gender, age, and dietary habits, minimizing irrelevant data.
- Prediction: The selected features are processed through multiple machine learning models (e.g., Logistic Regression, Support Vector Machine). Each model then votes, with the majority guiding the final prediction outcome.
For instance, a study involving 18,682 patients used 10-fold cross-validation to ensure robust testing of the prediction model, ultimately achieving an accuracy of 97.1% (Nature, 2025).
Practical Examples and Implications
Consider a healthcare provider using the obesity risk framework to assess patients’ risk based on gathered data. For instance, if a patient is a 35-year-old female with a sedentary lifestyle and a family history of obesity, the model can flag her as high risk and suggest targeted lifestyle interventions. Such a proactive approach has implications not only for individual healthcare but also for public health policy and resource allocation.
Common Pitfalls and Solutions
One common pitfall in obesity risk prediction models is the bias introduced by uneven data representation. If certain demographic groups are underrepresented, the model may generate inaccurate predictions for those groups. To mitigate this risk, it’s vital to implement techniques such as stratified sampling during data collection to ensure diverse representation.
Another issue is overfitting, where the model performs well on training data but fails on unseen data. To avoid this, employing techniques like cross-validation and regularization is essential.
Tools and Frameworks in Practice
Several frameworks and algorithms enhance the prediction of obesity risk. For instance:
- EC-QBA has shown superior feature selection performance compared to traditional methods, optimizing accuracy to 96% (Nature, 2025).
- SHAP (SHapley Additive exPlanations) can assess the significance of model features, thus improving interpretability and aiding in clinical decisions.
Many healthcare institutions implement these tools during patient assessments, especially in research settings where accurate predictive models can inform interventions and policy.
Variations and Alternatives in Methodologies
Alternative approaches to obesity risk prediction include traditional statistical methods like regression analysis, which lacks the ability to capture nonlinear relationships in complex datasets. While simpler models may be less computationally intensive, they often result in lower accuracy. The choice of method should depend on the specific data characteristics and the required outcome—whether high accuracy or interpretability is prioritized.
Regarding feature selection algorithms, while EC-QBA offers significant predictive advantages, other methods like Recursive Feature Elimination or Principal Component Analysis may serve well in specific scenarios, especially when computational resources are limited.
FAQ
What datasets are commonly used for obesity risk prediction?
Datasets often include demographic, behavioral, and lifestyle data collected through surveys. For instance, a popular dataset from Kaggle features over 20,000 entries with several relevant attributes (Kaggle, 2025).
What machine learning models are preferred for maximizing prediction accuracy?
Ensemble methods like Random Forest and Gradient Boosting Machines are typically favored for their ability to combine multiple models, which often leads to higher accuracy compared to single models.
How can practitioners interpret machine learning results for obesity risk?
Using tools such as SHAP, practitioners can gain insights into how different features contribute to predictions, guiding both clinical interventions and patient discussions.
Is the proposed framework scalable for larger datasets?
Yes, the population-based architecture of techniques like EC-QBA inherently supports scalability, allowing the model to handle increasing data complexity effectively. However, continuous evaluation on diverse datasets is necessary to ensure reliability.