“Validating a Deep Learning Tool for Assessing Spinopelvic Mobility in Total Hip Arthroplasty”
Validating a Deep Learning Tool for Assessing Spinopelvic Mobility in Total Hip Arthroplasty
Core Concept and Importance
Spinopelvic mobility refers to the dynamic relationship between the spine and pelvis during movement. It plays a vital role in surgical planning for total hip arthroplasty (THA), as misalignment in this area can lead to complications after surgery. Recent advances in deep learning (DL) are providing new methods for accurately assessing this relationship, helping surgeons make better-informed decisions for their patients.
Key Components of Spinopelvic Mobility Assessment
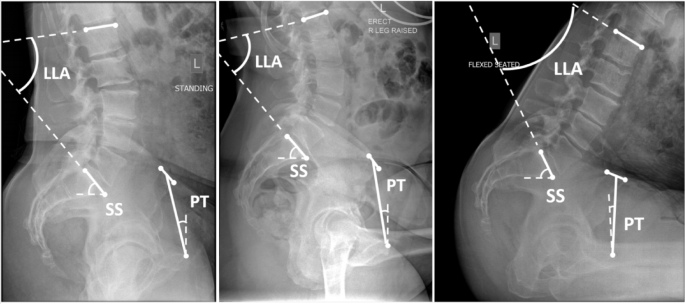
The evaluation of spinopelvic mobility involves three key parameters: Pelvic Tilt (PT), Sacral Slope (SS), and Lumbar Lordotic Angle (LLA). PT measures the angle formed by a line from the anterior superior iliac spine to the pubic symphysis against a vertical line. SS assesses the angle between the sacral endplate and a horizontal line. LLA quantifies lordosis in the lower spine. Understanding these parameters is essential for accurate surgical planning.
The Deep Learning Process
Building a robust DL model for evaluating spinopelvic parameters involves several steps. The first step is data collection, which can include radiographs and other imaging modalities. In this study, lateral functional imaging was retrieved from a large international registry comprising over 38,000 THA cases.
Once the data is collected, the next step is preprocessing. For example, medical images are often converted to a standardized format, and pixel intensities are normalized to prepare the data for analysis. Following this, a DL model, such as a Vision Transformer or CNN, is trained to detect landmarks in the X-ray images.
Practical Example: Case Study
In a recent study, researchers applied a DL pipeline to classify lateral functional radiographs into three functional positions: standing, flexed seated, and contralateral step-up. This classification is crucial for then calculating PT, SS, and LLA. The study employed a substantial dataset sourced from 391 imaging centers across multiple countries, allowing for diverse and comprehensive training.
Common Pitfalls in Implementing Deep Learning
When deploying DL for medical imaging, several challenges can arise. For instance, variations in image protocols across different centers can lead to inconsistencies in model performance. To mitigate these risks, a robust preprocessing pipeline was initiated to standardize the input images before they could be used for training, validation, and testing. Additionally, utilizing extensive data augmentation techniques helps create a more versatile model that can handle different imaging scenarios.
Tools and Frameworks Utilized
The DL pipeline in this study employed various advanced tools and frameworks. The Vision Transformer was used for initial image classification, while YOLOv8 handled the detection of individual vertebrae. For landmark detection, a convolutional neural network (CNN) was put to work. Each of these components was carefully designed to enhance the accuracy and efficiency of spinopelvic parameter calculation.
Variations and Trade-Offs
While deep learning holds significant promise for sensory analytics in healthcare, it’s essential to consider alternative methodologies. For instance, traditional statistical models or simpler machine learning techniques could be employed, though they may not achieve the same level of accuracy. The trade-off here often comes down to the complexity of implementation versus the reliability of results; DL methods require more data and computational power but generally produce superior outcomes.
FAQ
Q: How is deep learning enhancing the assessment of spinopelvic mobility?
A: Deep learning automates the identification of critical landmarks in imaging, potentially reducing human error and improving surgical outcomes.
Q: What makes this DL model clinically relevant?
A: The model’s accuracy in predicting spinopelvic mobility directly impacts surgical planning, leading to a lower rate of postoperative complications.
Q: Are there any limitations to using DL for this purpose?
A: Yes, the effectiveness of DL models may vary based on the quality and quantity of data, as well as the consistency of imaging protocols across different centers.
These insights into deep learning’s role in assessing spinopelvic mobility in THA provide a compelling look at how technology can enhance surgical precision. Innovations in this field promise not only improved patient outcomes but also more streamlined surgical processes, paving the way for future research and application in orthopedic surgery.