“Predicting Depression in Older Adults with Non-Communicable Diseases in India Using Machine Learning”
Application of Machine Learning Models for Predicting Depression Among Older Adults with Non-Communicable Diseases in India
Understanding the Core Concept
The intersection of machine learning (ML) and mental health is opening new avenues for early diagnosis and treatment. For older adults battling non-communicable diseases (NCDs) like diabetes and hypertension, the risk of depression escalates significantly. In India, an emerging body of research is applying ML techniques to predict depression in this vulnerable demographic. This predictive capability could inform interventions tailored to individual needs, optimizing mental health outcomes.
Key Components of Depression Prediction
Recognizing depression in older adults involves understanding various predictors. Variables contributing to depressive symptoms can be demographic (e.g., age, gender), health-related (e.g., chronic diseases, self-rated health), and lifestyle factors (e.g., physical activity, social engagements). For instance, research indicates that older adults suffering from multiple chronic conditions face a higher risk of depression compared to those with fewer health issues (UN, 2023).
Moreover, tools like Random Forest and Support Vector Machines (SVM) can process this multifaceted data to pinpoint patterns and correlations indicative of depression. The depth of analysis provided by these models is often unattainable through traditional statistical methods.
Step-by-Step Process of Implementation
-
Data Collection: This encompasses gathering demographic, health, and lifestyle data from older adults with NCDs. Surveys and electronic health records serve as primary data sources.
-
Feature Selection: Not all variables hold equal importance. Using methods such as Information Gain, researchers can identify key features relevant to predicting depression.
-
Model Training: Various ML models, including Random Forest, KNN, and Logistic Regression, are trained on a portion (e.g., 70%) of the dataset. Each model learns to identify features associated with depression.
-
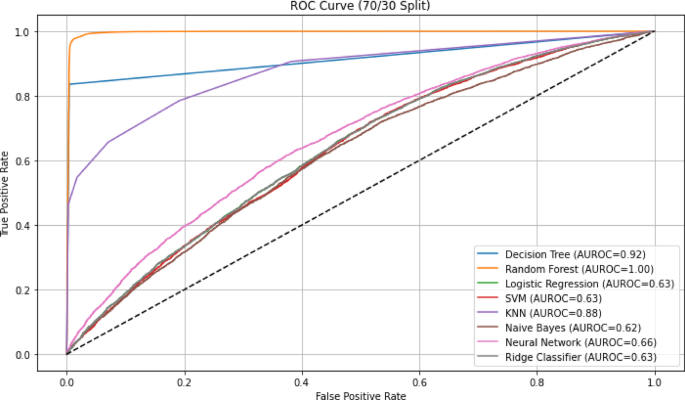
Model Evaluation: The remaining data (30%) is utilized for testing model performance through metrics like accuracy, sensitivity, specificity, and AUC-ROC curves. Strong models will exhibit high predictive power while minimizing false positives.
- Implementation: Finally, the most effective model is deployed in clinical settings, aiding healthcare professionals in diagnosing and handling mental health issues.
Practical Examples: Case Mini-Study
In a recent study involving older Indian adults, various ML models were evaluated to predict depression. The Random Forest model emerged as the frontrunner, achieving an accuracy of 95.6% and an AUC-ROC score of 0.996. This suggests that it outperforms conventional methods in terms of both sensitivity and specificity (Nature, 2023).
For instance, individuals who reported poor sleep and high body mass index (BMI) were identified as being at elevated risk for depression. This type of targeted screening can allow health providers to tailor interventions, such as sleep hygiene education or nutritional counseling, aimed at reducing depressive symptoms.
Common Pitfalls and How to Avoid Them
While implementing ML models in healthcare, several pitfalls can arise:
-
Overfitting: This occurs when a model becomes too complex and begins to model the noise rather than the signal. Utilizing techniques like cross-validation can mitigate this risk.
-
Bias in Training Data: If the data used to train models isn’t representative of the target population, predictions can be skewed. A diverse dataset is crucial for reliable outcomes.
- Interpretability: Some models, particularly neural networks, can act as black boxes, making it hard to interpret their predictions. Models with greater interpretability, like decision trees, should be emphasized, especially when human factors are involved in health decisions.
Tools, Metrics, and Frameworks in Practice
The study of predicting depression in older adults employs several tools and frameworks:
-
ML Libraries: Tools such as Scikit-learn and TensorFlow allow researchers to build, train, and evaluate various models efficiently.
- Metrics for Evaluation: Key performance metrics include:
- Accuracy: The proportion of true results among the total number of cases.
- AUROC (Area Under the Receiver Operating Characteristic Curve): Indicates how well the model distinguishes between classes.
- F1 Score: Balances precision and recall, particularly useful in imbalanced datasets.
Variations and Alternatives with Trade-offs
Numerous ML models exist, each presenting its unique advantages and trade-offs. For instance, while Random Forest offers high accuracy and handles non-linear relationships well, it may lack interpretability when compared to simpler models like Logistic Regression. Hence, the selection of appropriate models must align with the intended outcomes, balancing complexity with transparency.
FAQ
Q: What role does data privacy play in using ML for health predictions?
A: Data privacy is paramount, especially in health applications. Adhering to regulations like GDPR and ensuring anonymization of patient data can help safeguard sensitive information.
Q: How do these predictive models get refined over time?
A: Continuous data collection and feedback allow models to be retrained periodically, enhancing their accuracy and relevance as new patterns and trends emerge in healthcare outcomes.
In essence, the application of machine learning in predicting depression among older adults with non-communicable diseases opens new doors to precision medicine, potentially transforming the landscape of mental health support in India.