Understanding the Journey of Ethics Approval in Clinical Research
When embarking on clinical research, particularly studies involving human participants, ethics approval is a crucial step. This process ensures that the rights, dignity, and well-being of participants are protected, aligning research endeavors with moral and ethical principles. In this article, we explore the journey of ethics approval, using a recent study from Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, as a case in point.
The Significance of Ethics Approval
Ethics approval serves as a safeguard for participants, ensuring that their participation in research projects is voluntary and informed. This requirement is guided by the Declaration of Helsinki, which emphasizes respect for individuals and the necessity for ethical review. In the aforementioned study focusing on thyroid cancer, the researchers obtained approval from the local Ethics Committee and the Institutional Review Board (IRB), thus adhering to ethical standards.
Retrospective Data Collection
The research employed retrospective data collection, which entailed gathering information from patients diagnosed with thyroid cancer. This method allows researchers to analyze previously collected data without actively recruiting new participants, which can often expedite the research process. In this particular study, researchers collected demographics, operative procedures, pathology reports, and complications of patients who underwent thyroidectomy.
Exemption from Informed Consent
One notable aspect of the study was the exemption from obtaining informed consent from patients and controls. The IRB granted this exemption due to the retrospective nature of the study. Such decisions are typically made to ensure that unnecessary barriers do not impede valuable research that could benefit patient outcomes in the long run.
Establishing Inclusion and Exclusion Criteria
To maintain rigor and accuracy, the study defined clear inclusion and exclusion criteria. Eligible participants were those aged 18 or older, who had clear ultrasound images related to their thyroid examination. Patients diagnosed with thyroid malignant nodules and who underwent central lymph node dissection were included, while those with missing pathological reports were excluded. This meticulous process ensures that the data is both credible and robust.
Image Quality Control
Image quality is a critical component in studies reliant on visual data. Researchers implemented strict control measures to ensure that images used were of high quality. This included excluding images that were poorly captured or contained ambiguous data. Researchers gathered extensive clinical information, including the Kwak Thyroid Imaging Reporting and Data System (Kwak-TIRADS) grades, to underpin their analyses.
Data Annotation and Quality Control
The study illustrated a two-step data annotation process to guarantee precision in identifying malignant nodules and assessing lymph node metastasis. Initially, independent ultrasound physicians reassessed images, seeking to resolve discrepancies with original reports. Then, specialized radiologists analyzed the correlation between ultrasound images and pathological assessments. This collaborative effort enhanced the accuracy of findings and bolstered the study’s integrity.
Multi-Hospital Cohorts
Another intriguing aspect was the collection of data from seven hospitals, creating both training and test cohorts. This broad approach helped to ensure that the research population was reflective of diverse communities across China. By having a valid sample that encompasses different geographical and ethnic backgrounds, the findings of the study are more likely to be generalizable.
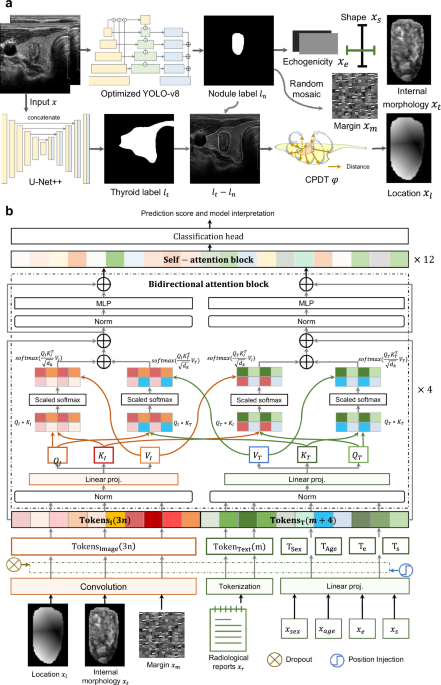
Advanced Predictive Models
Central to the study was the development of the LLNM-Net, a predictive model that utilizes machine learning to analyze the likelihood of lateral lymph node metastasis (LLNM) in thyroid cancer patients. The innovative model combined segmentation, distance transformation, and attention mechanisms, allowing it to integrate multifaceted data sources including ultrasound images and clinical reports.
Evaluation Methodology
The study employed rigorous evaluation methodologies to assess model performance, such as the Area Under the Curve (AUC) for receiver operating characteristic (ROC) analysis. Researchers also compared the predictive effectiveness of their AI model against human experts in diagnosing thyroid cancer and predicting LLNM. This comparison not only provides insight into the model’s efficacy but also highlights the value of human expertise even in an increasingly automated field.
Statistical Analysis for Validity
Lastly, to ensure the results were statistically sound, the researchers utilized bootstrapping techniques to estimate confidence intervals for their performance metrics. This approach is critical in academic research as it provides a method to gauge uncertainty in the results, enhancing the validity of their claims.
Protecting Participant Privacy
During this entire process, a central tenet remained the protection of patient privacy. Researchers were granted access solely to anonymized data, reinforcing the ethical commitment to safeguard sensitive information throughout the research lifecycle.
Conclusion
The ethics approval process is a cornerstone of clinical research, assuring that studies prioritize the well-being of human participants. The thoughtful implementation of procedures, as demonstrated in the study from Ruijin Hospital, showcases the commitment to ethical integrity in advancing medical knowledge. By understanding and respecting these processes, researchers can contribute to a landscape of responsible and impactful clinical research.