Study Design and Population in Critical Care Research
The utilization of extensive databases like the eICU Collaborative Research Database and the Medical Information Mart for Intensive Care (MIMIC-IV v. 2.0) serves as a foundation for insightful studies in critical care. These publicly accessible ICU databases, available upon request and compliance with ethical training, encompass diverse patient encounters that significantly contribute to our understanding of patient outcomes in intensive care settings.
Database Overview
The eICU Collaborative Research Database comprises over 200,859 patient unit encounters, involving 139,367 unique patients who were admitted to 335 ICUs across 208 hospitals in the United States from 2014 to 2015. This database is de-identified, containing vital sign measurements, demographic data, and diagnostic information pertaining to each patient’s ICU experience.
Data processing for this database utilized PostgreSQL and the widely-recognized Python library, pandas. The features included in any analysis are carefully detailed in supplementary tables, ensuring a transparent approach to data handling and analysis.
Defining the Myocardial Infarction Cohort
In our study, we specifically targeted a cohort of patients diagnosed with myocardial infarction (MI). This includes not only STEMI (ST-Elevation Myocardial Infarction) and NSTEMI (Non-ST-Elevation Myocardial Infarction) presentations but also those classified under acute coronary syndrome with confirmed myocardial damage. The inclusion criteria were meticulously defined using a comprehensive list of diagnosis strings and the corresponding ICD-10 codes, which can be further explored in the Supplementary Material.
By excluding patients without confirmed myocardial damage, particularly those presenting with unstable angina, our cohort genuinely reflects the complexities and realities of myocardial infarction cases. This specific focus enhances the relevance of our findings in clinical contexts concerning MI management.
Study Population and Methodology
The selection of participants was guided by solid methodological frameworks previously established in critical care research. We set our inclusion criteria to include adults aged 18 to 89 years with an ICU length of stay of no less than 5 hours. This filter served to exclude transient patients, thereby maintaining the integrity of our cohort.
A total of 26,218 patients constituted the final MI subcohort, from which we extracted essential diagnostic indicators that were entered within the first 5 hours of their ICU admission. To ensure data quality, we also excluded patients without any laboratory measurements or further diagnostic information beyond this timeframe.
Validation Through External Datasets
To bolster the robustness of our findings, we performed external validation using the MIMIC-IV database, which houses over 15,000 additional ICU patient records. Like the eICU database, MIMIC-IV is a de-identified dataset, drawn mainly from the Beth Israel Deaconess Medical Center, offering insights collected between 2008-2019. Our selection criteria mirrored that of the eICU database and ultimately helped us derive a sample of 1,143 ICU stays involving confirmed MI from a broader 76,938.
This dual-database strategy allows us to validate our findings across different critical care environments and ensure our models maintain generalizability even in varied clinical settings.
Features and Data Processing
Our processing of the databases followed a uniform workflow aimed at ensuring consistency and reliability across datasets. We extracted only those predictors that appeared in our earlier analyses, focusing on the most important variables as identified by our interpretability framework. This approach ensures that only the critical features are used, which not only maintains the robustness of our predictions but also enhances clinical relevance.
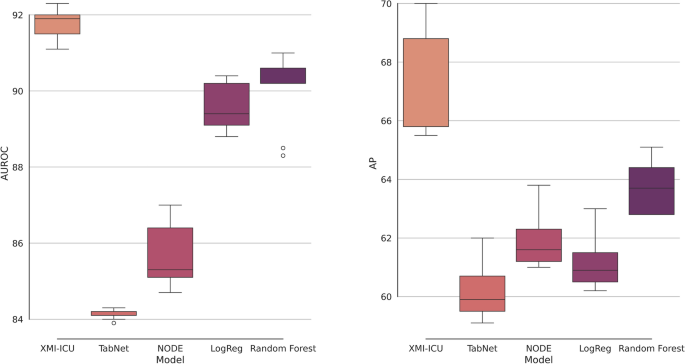
Models and Predictions
Employing machine learning models, we split the dataset into training and testing segments, ensuring a proportionate hold-out set for unbiased result reporting. Our methods involved hyperparameter tuning through Bayesian optimization and utilized strategies like inverse class-weighting to address the inherent class imbalances presented by mortality outcomes.
We also leveraged time-series analysis techniques to utilize vital sign data effectively. Through the implementation of rolling windows to capture patient data within specified timeframes, we created a framework that dynamically assesses mortality risk at various intervals following admission to the ICU.
Interpretability of Findings
A hallmark of our study is the introduction of a time-resolved Shapley value analysis, extending conventional interpretability measures. This innovative approach allows for real-time tracking of feature importance across different time windows, illuminating how predictions evolve as clinical conditions change. This is crucial for clinicians as it provides actionable insights on which indicators to monitor closely during critical illness progression.
Clinical Outcomes and Implications
Lastly, to comprehensively understand our model’s implications in clinical scenarios, we utilized decision curves to evaluate the effectiveness of our risk predictions. Such analysis goes beyond traditional metrics, assessing net clinical benefit and identifying the thresholds at which patient risk is accurately estimated—an essential concept for improving patient care in intensive medical settings.
The methodologies and frameworks outlined herein offer a solid foundation for ongoing research and practical application in the management of myocardial infarction patients in ICU environments, emphasizing the importance of rigorous data handling and interpretative clarity in clinical predictive modeling.