The Cost-Effectiveness of Machine Learning in Detecting Medial Vascular Calcification in CKD Patients
In a compelling study that evaluates the intersection of machine learning and healthcare, researchers have analyzed the cost-effectiveness of five machine learning frameworks designed to detect medial vascular calcification (mVC) in chronic kidney disease (CKD) patients—a demographic known for its heightened risk of mVC. With data compiled from 152 participants, the study uncovers valuable insights into statistical performance and cost-effectiveness ratios, offering a glimpse into the future of diagnostic processes.
Statistical Performance and Cost-Effectiveness Ratios
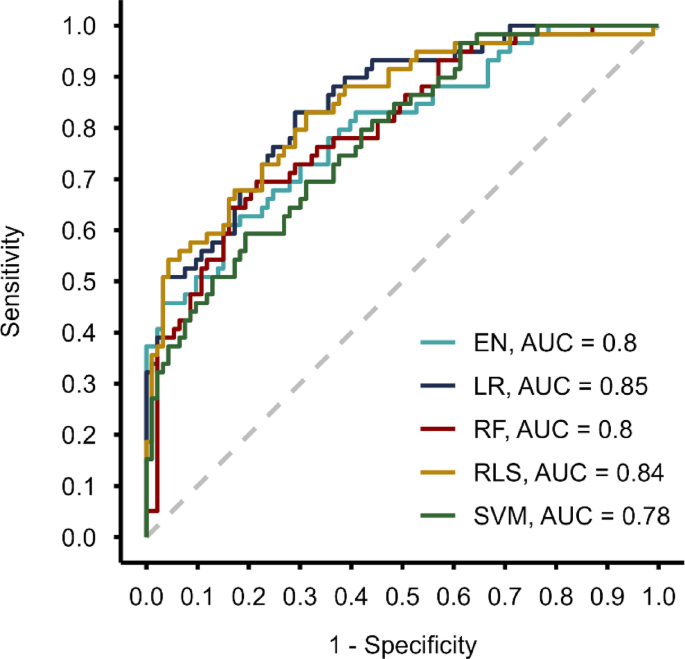
At the heart of the analysis is the Incremental Cost-Effectiveness Ratio (ICER), a vital metric that compares the cost and effectiveness of different health interventions. Each machine learning framework demonstrated similar predictive capabilities, yielding Area Under the Curve (AUC) values between 0.80 and 0.84. Interestingly, while the models effectively identified traditional risk factors such as age, diabetes, male sex, and body mass index (BMI), their effectiveness also varied when it came to mVC-related features.
Among the five frameworks assessed, Logistic Regression (LR) proved to be the most efficient option. By focusing on just five easily obtainable features, LR not only reduced the likelihood of encountering missing data, which is common in complex models, but also emerged as the best value option when considering cost-effectiveness.
Implications for Clinical Practice
The findings suggest that machine learning algorithms can serve as a valuable adjunct in clinical practice—particularly in reducing unnecessary CT scans. This potential benefit translates into significant savings in healthcare costs and minimizes both radiation exposure for patients and time spent on diagnostic procedures. However, it is imperative to remember that these algorithms should not be viewed as sovereign solutions; rather, they are aids in the broader context of clinical decision-making.
For instance, the study elucidated how adjusting the cut-off threshold for recommending scans could balance diagnostic accuracy against financial savings. Lowering the threshold might enhance accuracy but subvert the purpose of cost-saving measures. This nuanced balance underscores the importance of contextual decision-making in clinical practice, informed heavily by local healthcare resources and patient needs.
The Role of Biomarkers
Across the machine learning models, certain biomarkers emerged as particularly significant predictors of mVC. Copeptin was consistently selected across all algorithms, reaffirming its role as a critical biomarker associated with mVC. Other notable markers included osteoprotegerin and sclerostin, chosen by multiple models, further supporting previous research linking these biomarkers with vascular calcification.
Given the promising results of these biomarkers in predicting mVC, the study advocates for longitudinal research to determine whether integrating them into routine clinical assessments could enhance patient care. This calls for a reevaluation of standard diagnostic processes based on emerging scientific evidence.
Addressing Methodological Limitations
Despite the strengths of this comprehensive analysis, several limitations warrant consideration. Missing values in the dataset posed a challenge, yet the researchers opted for imputation to preserve statistical power. Nonetheless, the absence of external validation limits the generalizability of the findings, emphasizing the necessity for further validation studies.
Moreover, costs associated with the necessary measurements for ICER analysis can vary significantly, depending on geographical and laboratory factors. Thus, medical facilities contemplating the implementation of these machine-learning detection methods must evaluate their contextual resources for accurate cost assessment.
Understanding Vascular Bed Variability
The study’s findings also highlight variability in mVC distribution across different vascular beds, with previous research indicating higher median scores for coronary artery calcification when assessed in specific arteries. This complexity reinforces the notion that mVC is not a monolithic condition and that future inquiries should dissect how selected features impact calcification in various vascular regions.
Final Thoughts
Overall, the study captures the promising potential for machine learning frameworks coupled with predictive analytics in enhancing the detection of vascular calcification. The exploration of cost-effectiveness alongside statistical metrics serves as an essential contribution to ensuring that innovations in biomedical research align with practical clinical applications. As the landscape of healthcare continues to evolve, continuous evaluation of both risk factors and diagnostic methods will be crucial for improving outcomes in high-risk populations like CKD patients.