Understanding Osteoarthritis Progression: Insights from Recent Findings
Osteoarthritis (OA) is a complex and multifaceted condition that affects millions worldwide, leading to pain, stiffness, and mobility challenges. Recent research has shed light on how various factors influence the progression of OA, unveiling distinct patterns depending on bone mineral density (BMD) and the presence of osteophytes, among other factors.
The Relationship Between BMD and OA Progression
One of the standout findings from recent studies is the significant role of BMD in the progression of osteoarthritis. Patients with low BMD and a high osteophyte grade were shown to have a higher likelihood of progressing to tricompartmental OA. In contrast, individuals with high BMD and low osteophyte grades were more likely to develop unicompartmental OA.
This highlights a pivotal relationship: while lower BMD tends to correlate with more generalized forms of OA, higher BMD may drive the development of localized OA. The ongoing debate surrounding whether high or low BMD is associated with OA progression underscores the complexity of this condition.
Aging and Bone Density: Key Demographic Factors
Age and BMD interact to influence the progression of OA. Older patients with low BMD are particularly at risk of transitioning to tricompartmental joint space narrowing (JSN)-dominant OA. The deterioration of subchondral bone integrity due to osteoporosis likely contributes to this pattern. In older adults, weakened bone structure leads to increased stress on the cartilage, accelerating degeneration and the onset of symptoms in multiple compartments of the knee.
Conversely, younger individuals with metabolic diseases and higher BMD levels may exhibit progression towards unicompartmental OA. This points to potentially different underlying biomechanical stresses and biochemical processes affecting joints in younger patients compared to their older counterparts.
The Role of Metabolic Diseases
Metabolic diseases have emerged as influential factors in OA progression. Those with conditions such as obesity or diabetes risk exacerbating their OA symptoms. The relationship between metabolic disorders and OA likely stems from systemic inflammation and mechanical overload on the joints. Recent studies indicate that metabolic syndromes lead to increased synovial inflammation and bone density alterations, which can accelerate OA progression.
This relationship suggests a necessity for targeted treatments that consider a patient’s metabolic health as a significant component of OA management.
Machine Learning in Predicting OA Progression
Innovative approaches are being utilized to better predict OA progression. The use of machine learning (ML) models, specifically the LightGBM model, has shown promise in outperforming traditional logistic regression in predicting OA patterns. These models can analyze a multitude of factors—including demographics, comorbidities, and radiographic images—to discern which characteristics are most impactful in terms of progression.
By employing SHAP (SHapley Additive exPlanations) methodology, researchers can interpret these ML models to understand the contributing factors to OA classes better. This could pave the way for personalized treatment strategies based on individual risk profiles.
The Impact of BMI on Osteoarthritis
Body Mass Index (BMI) also plays a noteworthy role in OA classification. It was observed that the tricompartmental OA group generally reported higher BMI values compared to those with unicompartmental OA. This relationship may not be linear; instead, it suggests that a certain threshold of BMI contributes to a higher risk of knee OA. Beyond just mechanical loading, the systemic inflammation brought on by obesity may accelerate cartilage degradation.
The interplay between BMI and OA illustrates that while obesity can lead to mechanical overload on the knee joint, it may also initiate broader inflammatory processes negatively impacting joint health.
Distinguishing Between OA Phenotypes
The distinctions between unicompartmental and tricompartmental OA highlight the necessity for tailored interventions. Unicompartmental OA typically arises from localized biomechanical stresses, while tricompartmental OA often results from systemic factors like low BMD or osteoporosis. Recognizing these differences can inform more effective treatment options, potentially leading to better long-term outcomes.
Furthermore, early identification of specific OA phenotypes may allow clinicians to intervene proactively, using personalized strategies that could include alignment surgery for those with unicompartmental OA or osteoporosis treatments for tricompartmental OA patients.
Addressing Limitations and Future Directions
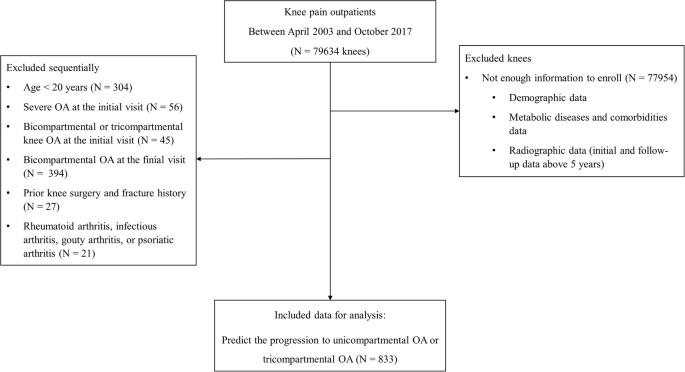
While these findings provide valuable insights into OA progression, it is crucial to acknowledge the limitations inherent in the studies conducted. For instance, data sourced from a single institution may restrict the generalizability of the results. The retrospective nature of the analyses may also introduce bias, particularly given variations in follow-up periods among patients.
Future studies should aim to involve larger, multicenter datasets that consider additional factors such as biomechanical influences, lifestyle variables, and a more balanced sex representation within the patient population.
Recapping the Multifaceted Nature of Osteoarthritis
The landscape of osteoarthritis progression is characterized by intricate relationships among BMD, age, metabolic health, and obesity. By exploring these connections and leveraging machine learning and comprehensive datasets, researchers and clinicians can work towards more targeted and effective interventions. Enhancing our understanding of the phenotypes of OA can ultimately lead to improved management strategies tailored to individual patients, potentially transforming OA treatment and prevention.