Understanding the Patient Population in Neuro-Intensive Care
Study Overview
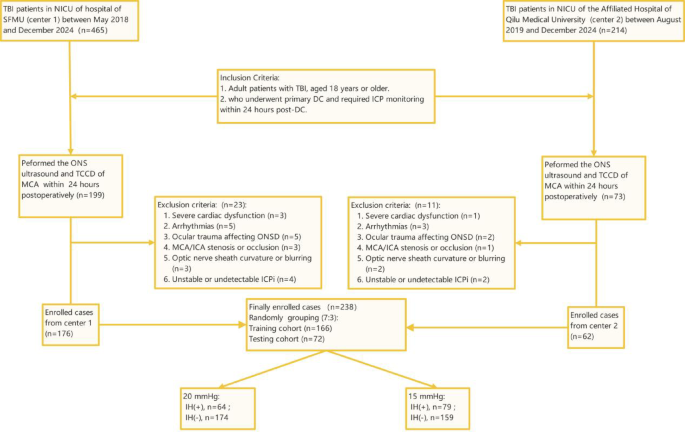
This retrospective observational study investigates a specific cohort of patients suffering from traumatic brain injury (TBI). Conducted in two prestigious neuro-intensive care units (NICUs)—at the Second Affiliated Hospital of Shandong First Medical University (SFMU) from May 2018 to December 2024, and at the Affiliated Hospital of Qilu Medical University from August 2019 to December 2024—the research emphasizes the clinical realities of managing TBI patients requiring a decompressive craniectomy (DC).
In a unique arrangement, the Ethics Committee of SFMU waived the necessity for informed consent, acknowledging the retrospective design of the study.
Patient Inclusion Criteria
The study included a total of 238 patients who met the stringent inclusion and exclusion criteria laid out in the research protocol. Specifically, participating individuals were adult patients aged 18 years or older, diagnosed with TBI, and who had undergone primary DC. Furthermore, these patients required intracranial pressure (ICP) monitoring within 24 hours postoperatively. The inclusion of young and elderly adults provided a broad understanding of the impact of DC across various age demographics.
Exclusion Criteria Details
While 238 patients were considered, several were excluded based on defined criteria. Patients with suboptimal TCCD (transcranial color Doppler) window quality, which hindered reliable 2D imaging, were not included. This criterion specifically affected individuals with significant cardiovascular or cerebrovascular conditions that could interfere with the reliability of the data. For instance, severe arrhythmias, critical valvular stenosis, and notable fluctuations in ICP were grounds for exclusion. Ultimately, 176 patients from SFMU and 62 patients from Qilu Medical University met all the necessary criteria and were divided into training and testing cohorts at a ratio of 7:3.
Treatment Protocols for TBI Patients
In this cohort, the management and treatment approaches for TBI patients were both intricate and standardized. The decision to perform primary DC hinged on various factors: the mechanism of injury, clinical symptoms, Glasgow Coma Scale (GCS) score, and the results of CT imaging. The surgical technique varied according to the nature of the lesions; unilateral DC was favored in cases with localized hematomas, while bilateral or frontotemporal decompression was indicated for more complex presentations.
The surgical intervention involved creating a bone flap, approximately 9 x 9 cm, to gain access to the dura mater. Postoperatively, continuously monitoring ICP was crucial, conducted via an intraparenchymal sensor or a ventricular catheter.
Intracranial Pressure Management
The study adhered to the Chinese Expert Consensus on Monitoring and Management of Elevated ICP, maintaining optimal cerebral perfusion pressure (CPP) between 60 and 70 mmHg. Various medications were applied, including sedation agents like propofol for burst suppression. Hyperosmolar therapies also played a key role—employing both 3% hypertonic saline and mannitol to manage severe ICP elevations. Therapeutic hypothermia was introduced for its neuroprotective properties, closely monitored to prevent rebound ICP elevation following rewarming.
Ultrasound Imaging and Methodologies
Ultrasound imaging of the optic nerve sheath (ONS) was a cornerstone of evaluation, performed twice within 24 hours post-DC using the Mindray M9 ultrasound system. This technique allowed for the assessment of ONS diameter, offering insights into ICP levels. Careful attention was given to probe frequency, power output, and imaging depth to capture high-quality images while adhering to safety guidelines.
In tandem, assessments were made using TCCD to evaluate middle cerebral artery (MCA) hemodynamics. Key parameters measured included peak systolic velocity (PSV) and end-diastolic velocity (EDV), critical for understanding cerebral blood flow amidst the injury.
Expertise in Imaging
The imaging assessments were performed by two ultrasound specialists with varying years of expertise—four and fifteen years, respectively. Both specialists underwent standardized training to ensure a uniform approach to measurements, and consensus discussions were held to resolve any discrepancies in their evaluations.
Radiomic Analysis
The study did not merely stop at visual inspection; it employed advanced radiomic techniques. Features were extracted from segmented regions of interest (ROIs) using PyRadiomics. These encompassed geometric, intensity, and texture categories that provided a comprehensive understanding of the ONS characteristics.
Deep Learning Methodologies
To further refine the analysis, a ResNet101 convolutional neural network was adapted for extracting deep transfer learning (DTL) features. DTL features from separate imaging modalities—ONS images and MCA assessments—were combined to create a robust representation of the data.
Statistical Rigor
Statistical analyses were conducted using MedCalc and Python, employing methods such as the Mann–Whitney U test for continuous variables and the chi-square test for categorical variables. With a standard significance level set at p < 0.05, the findings were statistically validated, reflecting the reliability and robustness of the results.
Throughout the study, emphasis was placed on multidimensional monitoring of patient health, dynamically adjusting treatments based on data to balance clinical efficacy with inherent risks associated with TBI management. The comprehensive approach showcased within this study offers immense insights—both valuable and applicable—in the continuous quest for optimized care in neuro-critical settings.